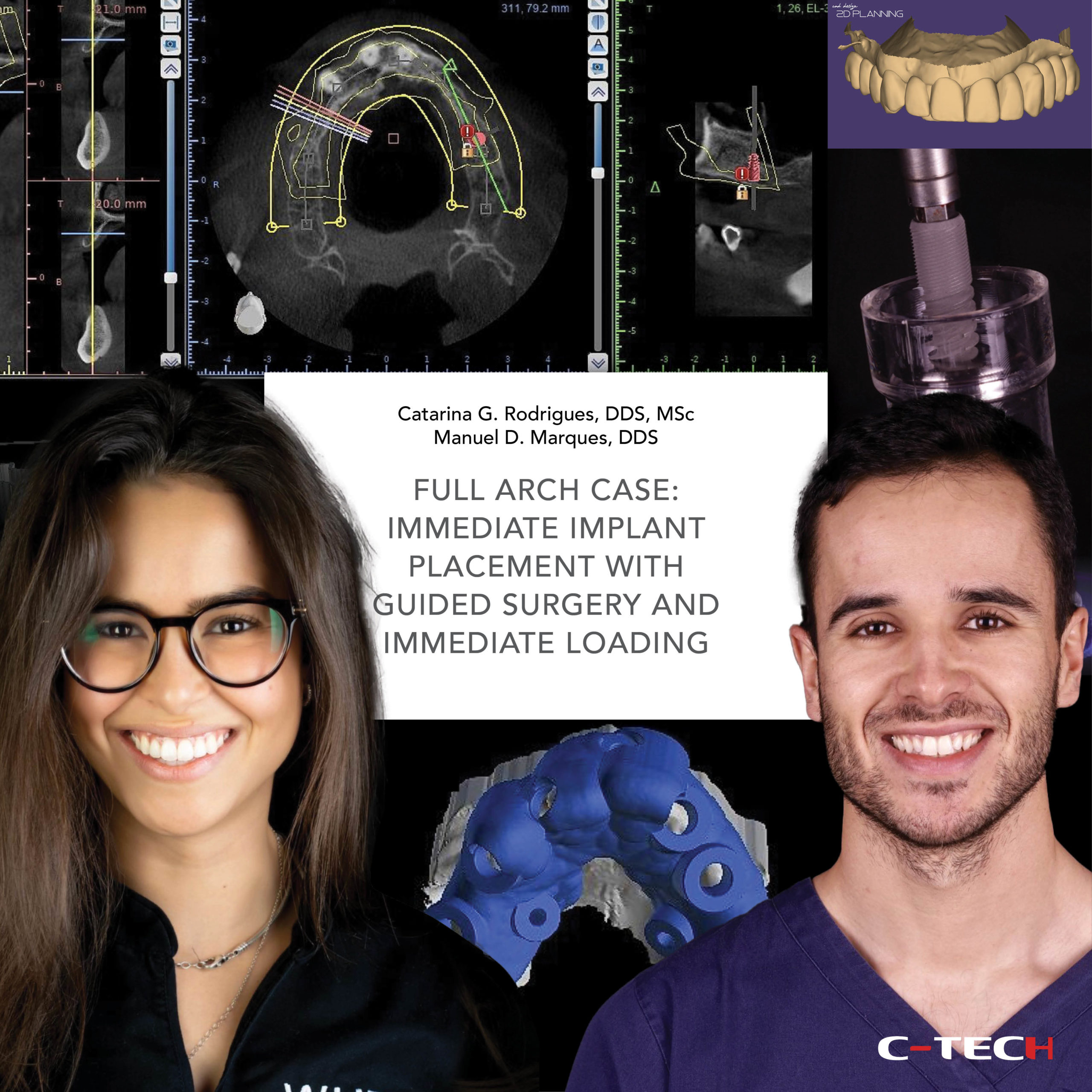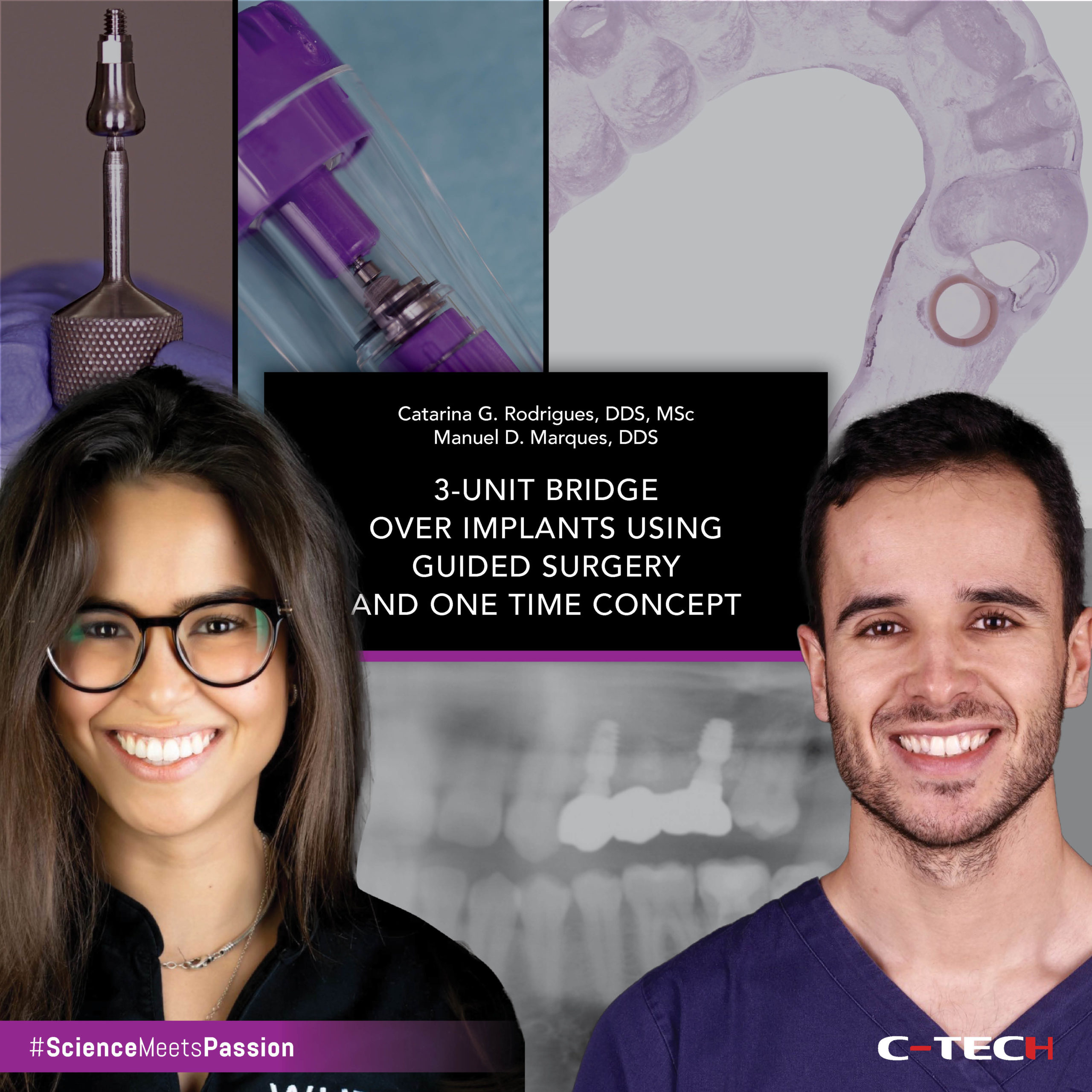
Dr. Catarina G. Rodrigues, DDS, MSc – Dr. Manuel D. Marques, DDS
One of the main challenges during implant treatment is adequate maintenance of peri-implant soft tissues. This will have a tremendous influence on the longevity of the implant, and aesthetics of the final implant-supported restoration.
In some clinical situations, the shape of pre-fabricated healing abutments is not adequate to obtain a proper emergence profile, as they differ from the shape of the natural tooth. That will happen most of the times when placing immediate implants, right after a tooth extraction.
The use of a custom healing abutment, not only will preserve the natural soft tissue architecture, but will also, later on, facilitate the work of the restorative dentist and lab technician on the fabrication of the final crown, as the soft tissue is already developed to accept a crown with a natural size and contour (Fig. 1).
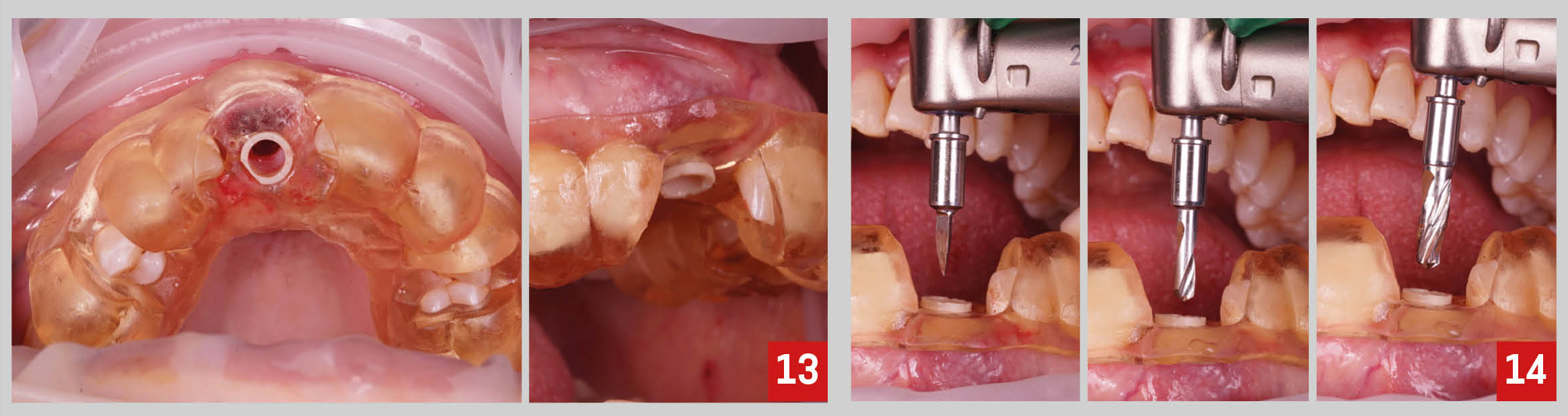
The present clinical case illustrates how to obtain a custom healing abutment using a temporary metal abutment and light-cured flowable resin composite (Fig. 2,3).

For this clinical situations, there are mainly three reasons for choosing a metal abutment over a peek one. First, the metal connection is stronger. Given the fact that we will need to screw and unscrew the abutment several times, by using an abutment with a stronger implant connection there is less risk of deforming it. Second, the surface characteristics and design of the metal temporary abutment facilitate the process of adding and retaining the resin composite. Lastly, when using the temporary metal abutment it is possible to confirm with a periapical x-ray the position of the abutment on the implant, while with peek abutments that will not be possible.
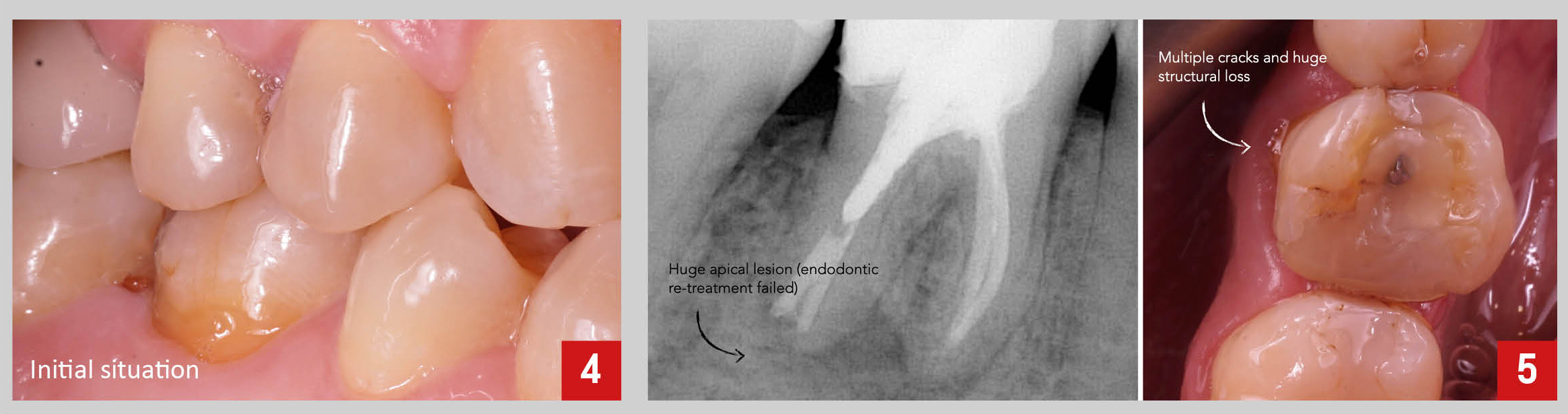
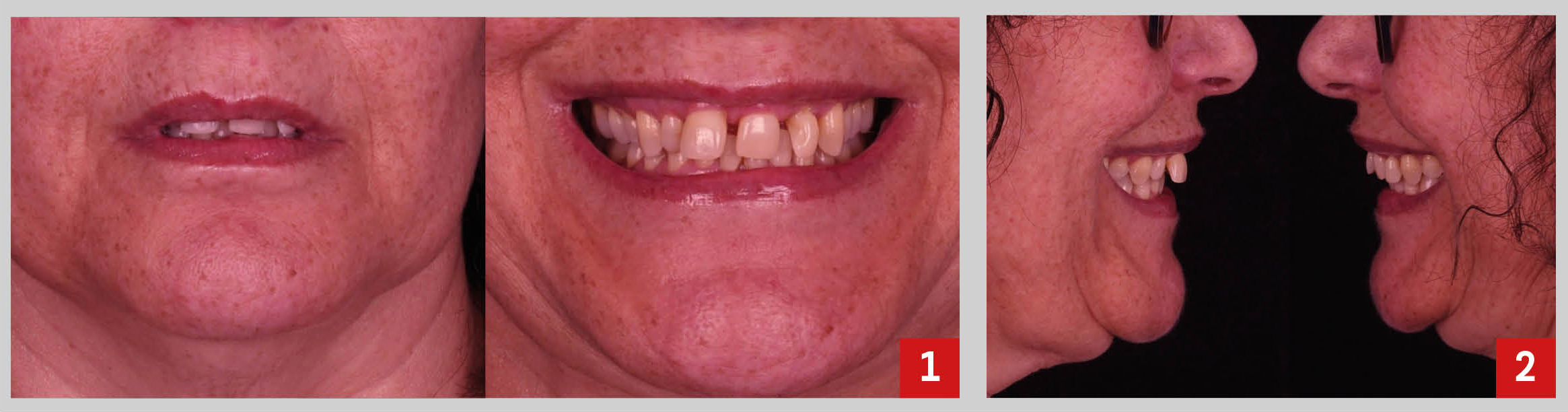
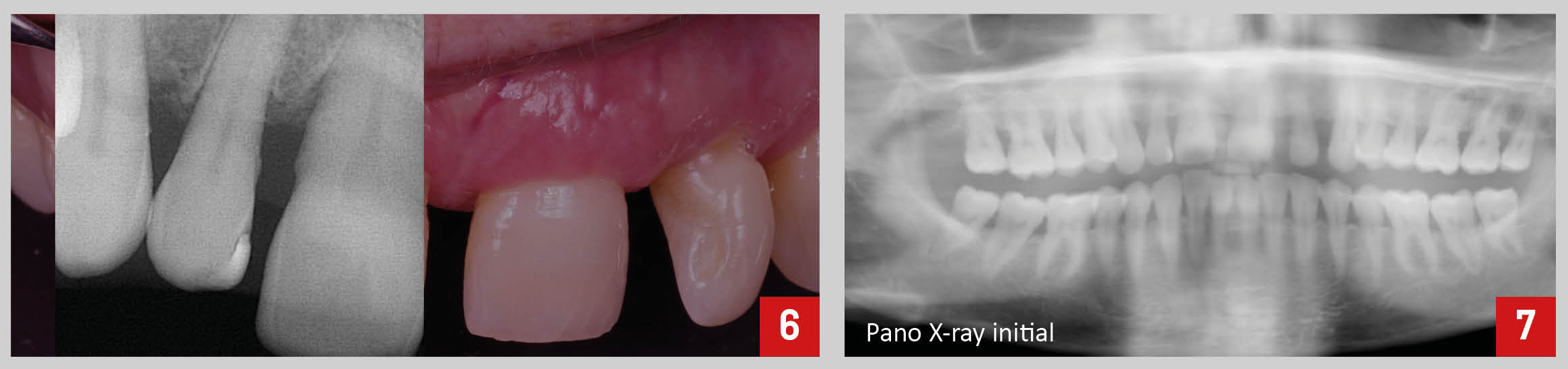
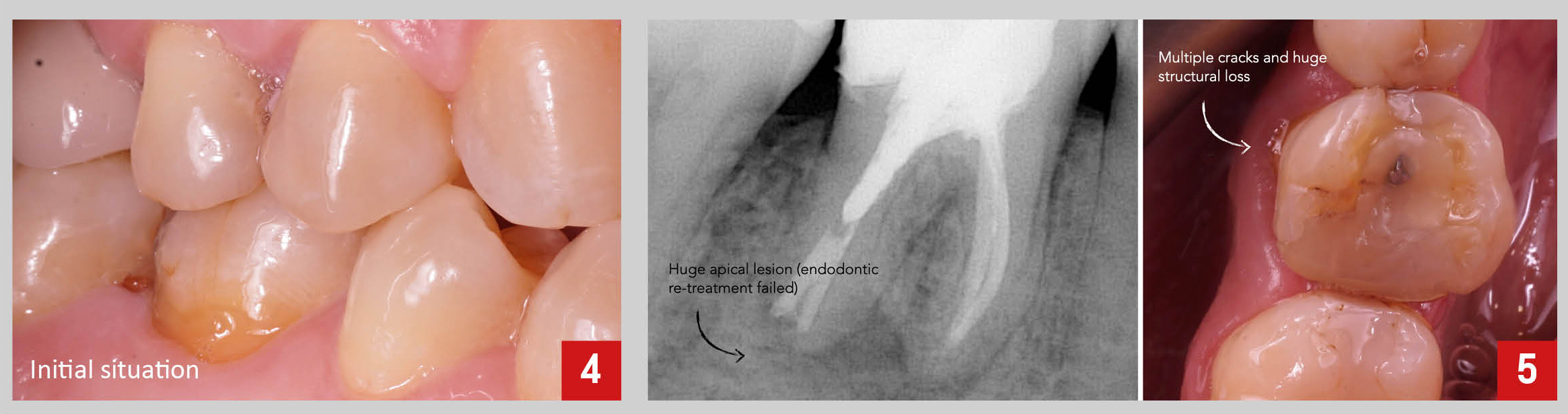
The patient presented with complaints on tooth 4.6. After a proper clinical and radiographic examination, a large apical cyst was found, besides signs of failed endodontic treatment, extensive structural loss and multiple cracks (Fig.4,5).
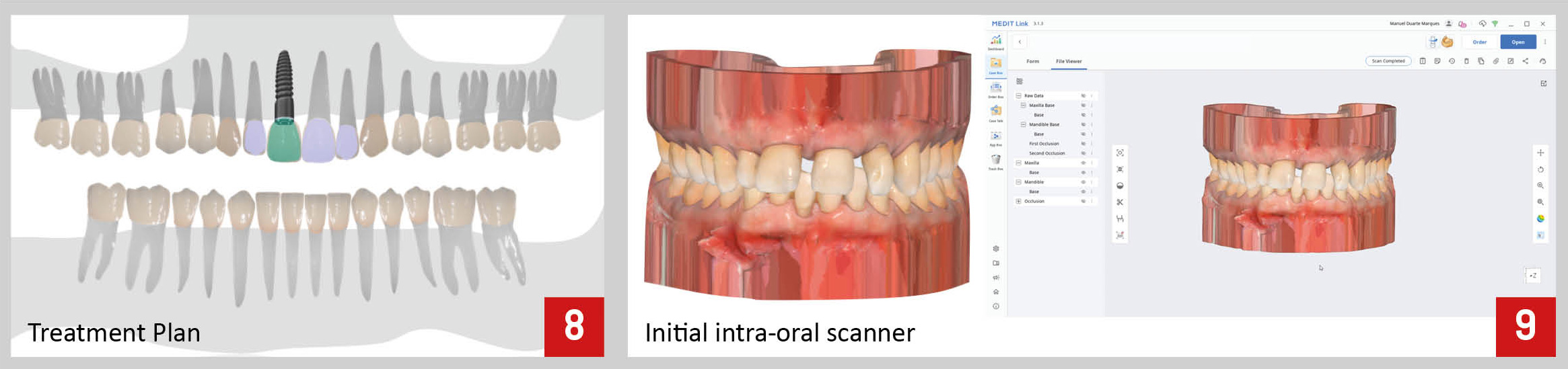
Given that the tooth was considered to have an unfavorable long-term survival, extraction and immediate implant placement was recommended as the ideal treatment plan.
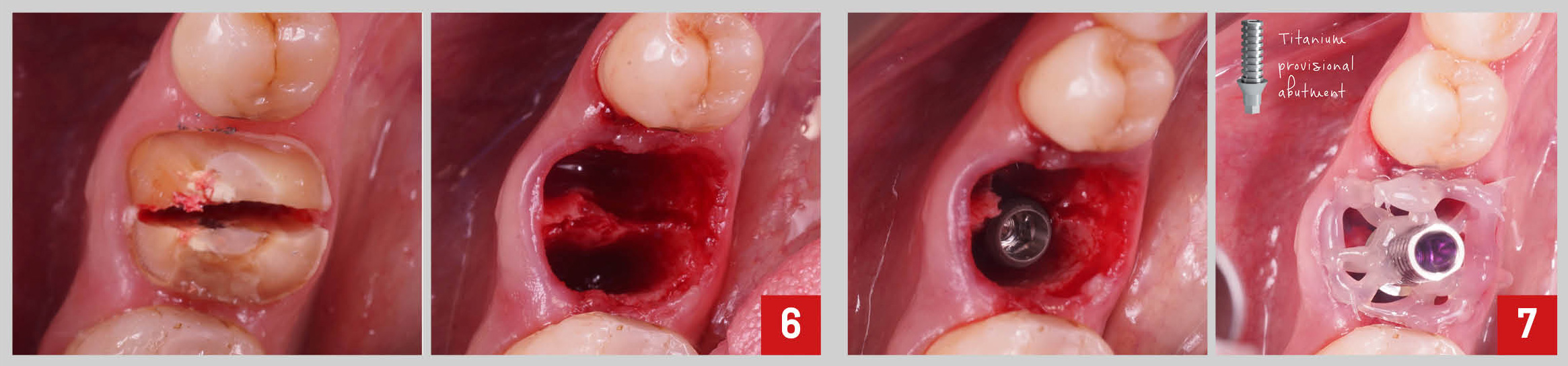
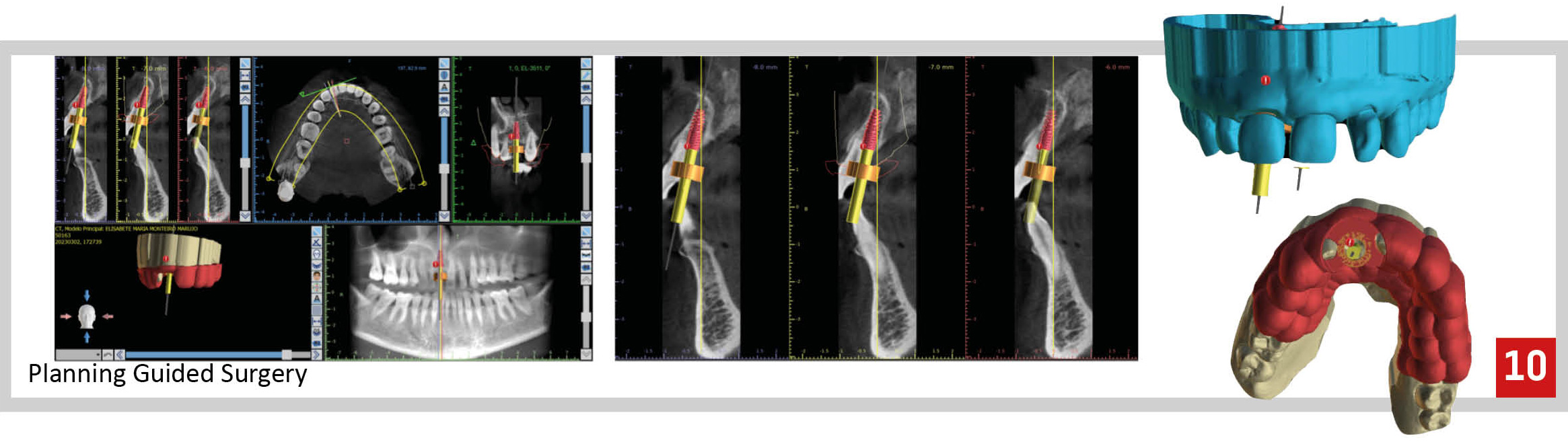
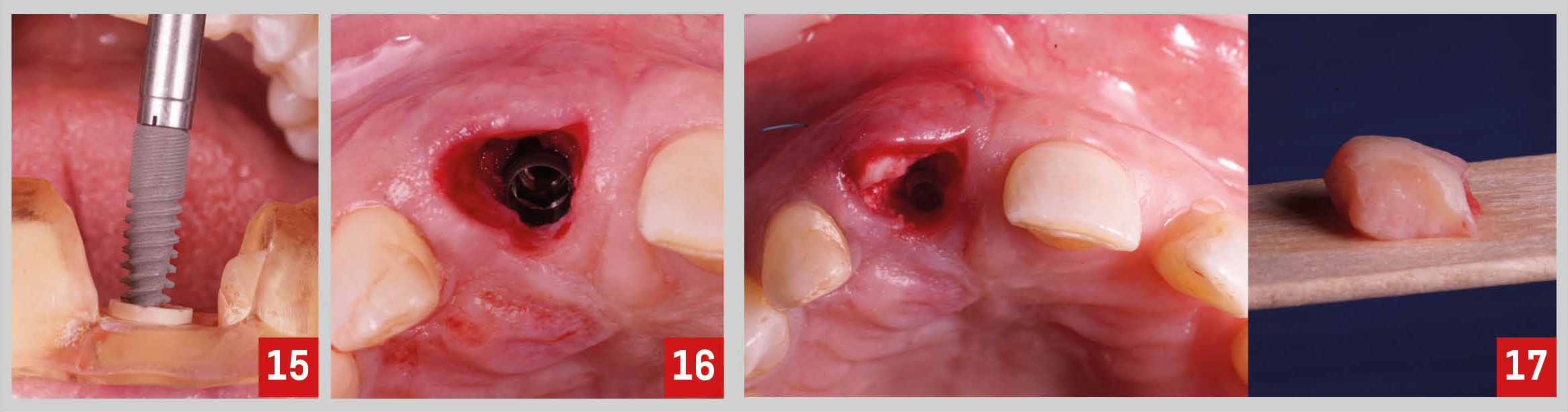
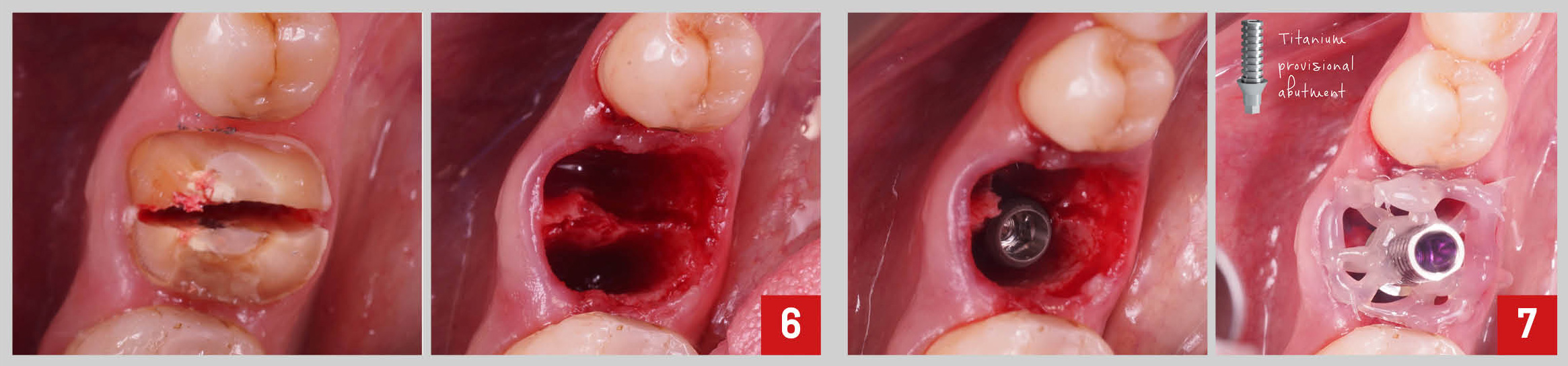
The surgical procedure consisted of atraumatic extraction of tooth 4.6, followed by immediate implant placement (Fig.6,7).
Then, a temporary metal abutment was screwed on the implant and the flowable resin composite was attached to the abutment, creating a “spider web” to help on reproducing the shape of the extraction socket to the design of the custom healing abutment (Fig.7).
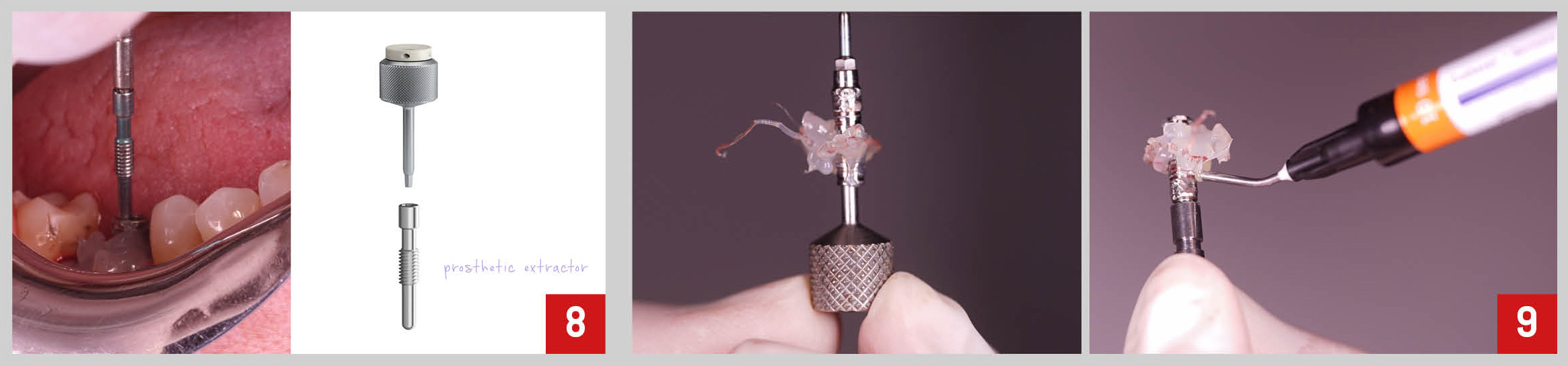
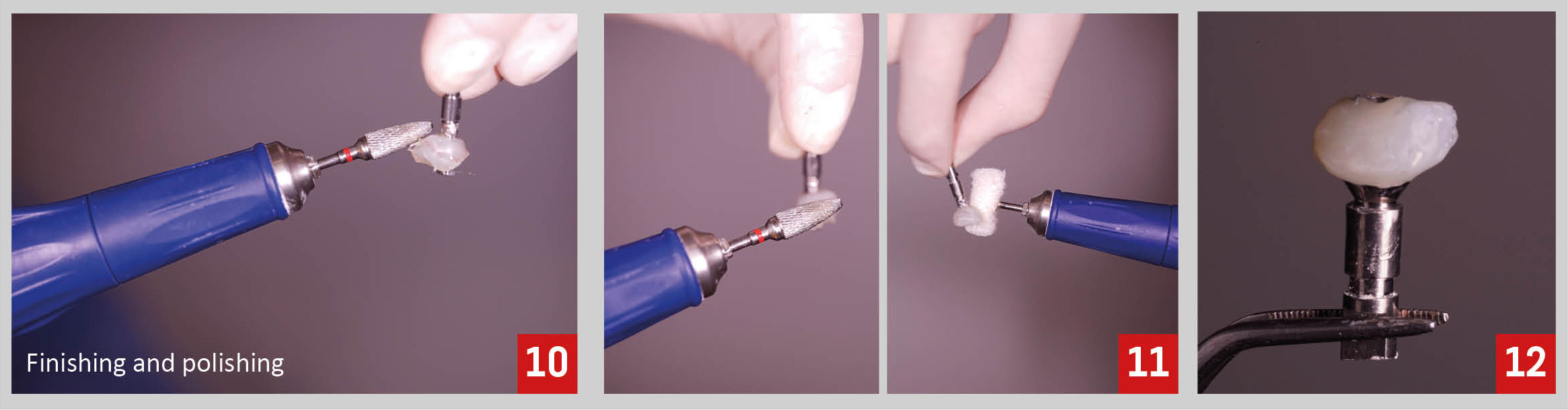
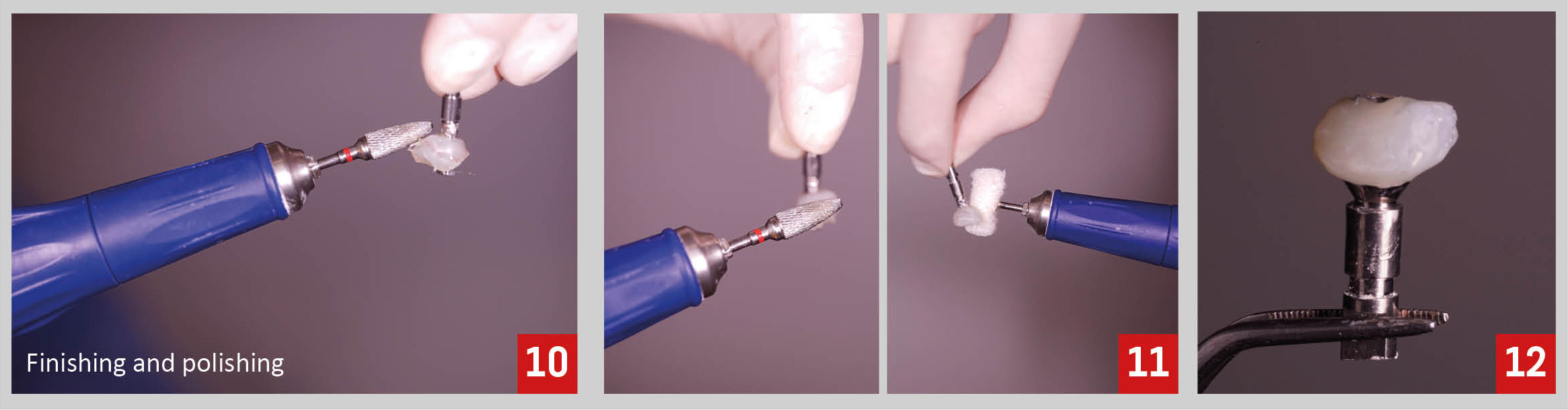
Then, the abutment was unscrewed (Fig.8), more flowable composite was add, within the limits previously defined, to create a proper emergence profile (Fig.9), and the finishing and polishing procedures were undertaken (Fig 10-12). 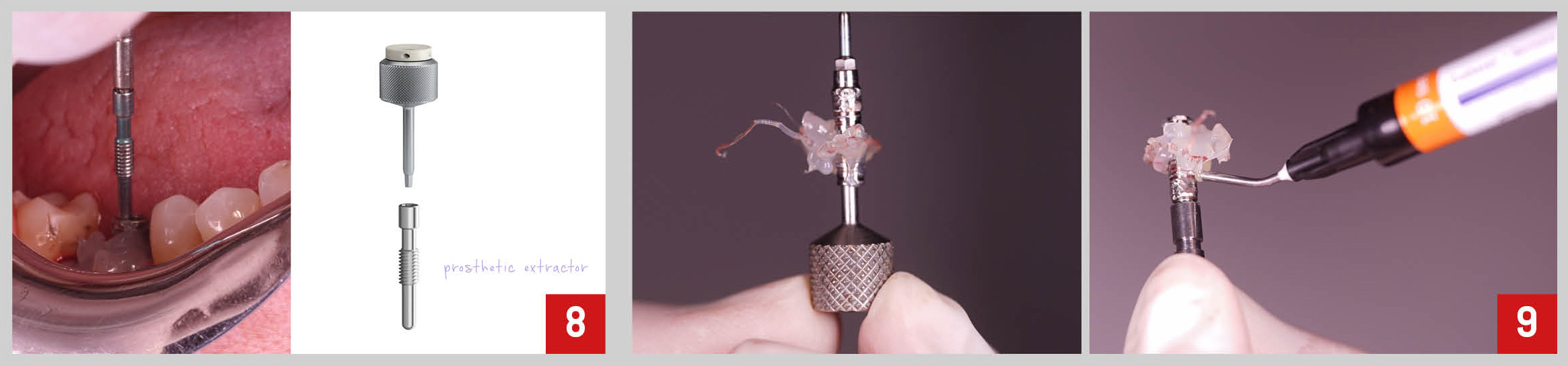
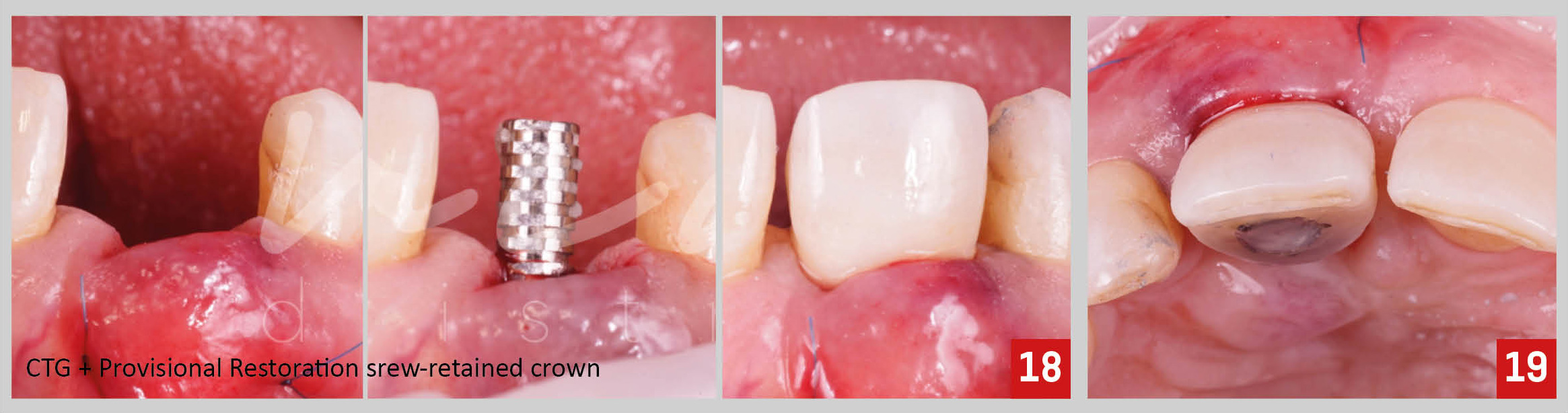
Finally, the socket was filled with a xenograft bone substitute and the custom healing abutment was screwed on the implant. No sutures were necessary as, due to its shape, the abutment itself closed the socket completely (Fig.13-15).

At one week post-operative control appointment we could appreciate a proper healing of the tissues (Fig. 16).
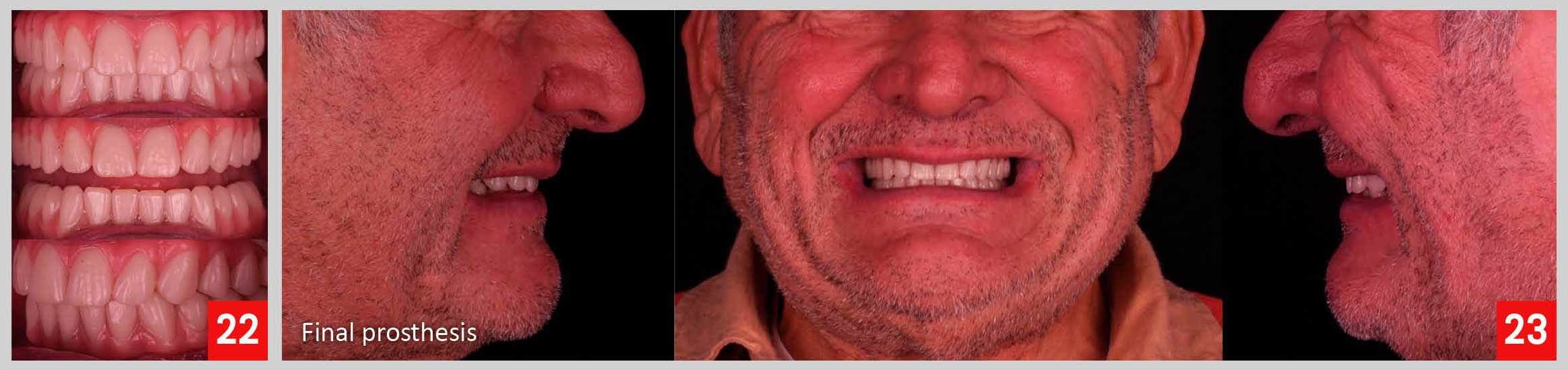
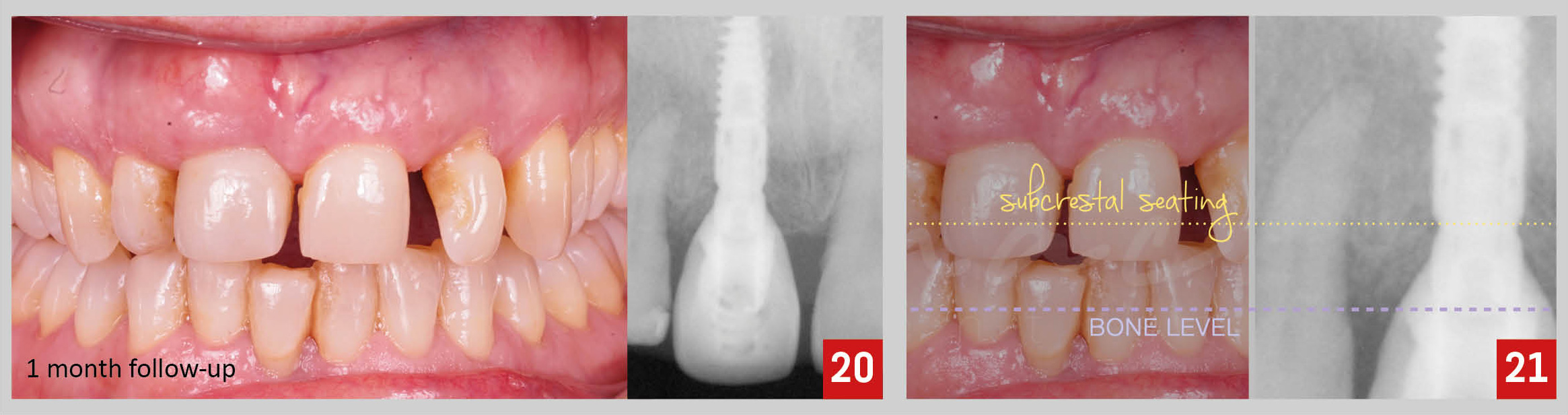
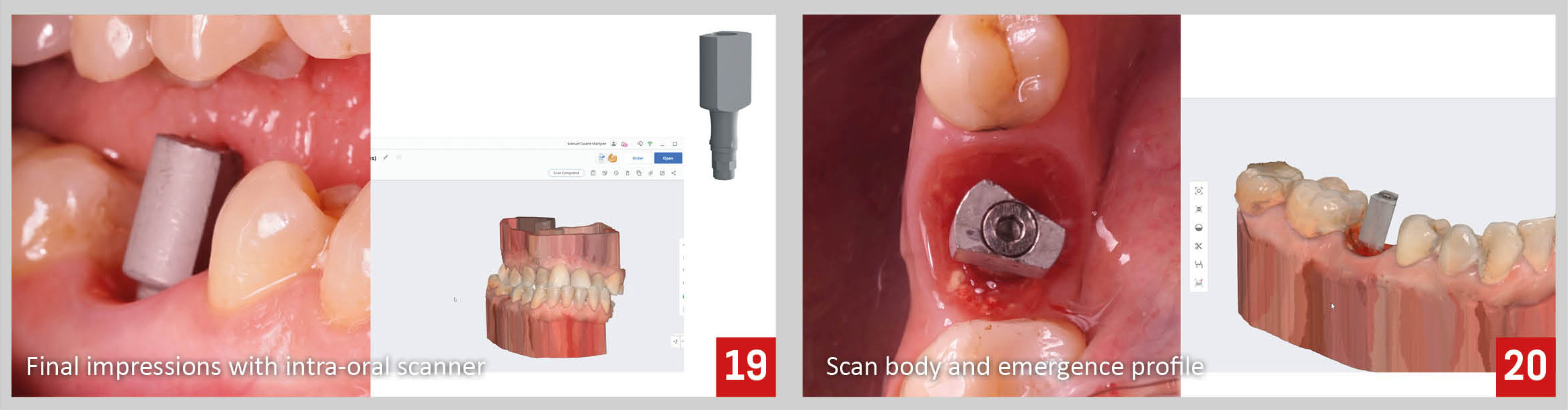
Three months after implant placement, we proceed with the final impressions. After removing the custom healing abutment, we can observe the maintenance of soft tissue contour thanks to the shape of the abutment itself (Fig.17,18).

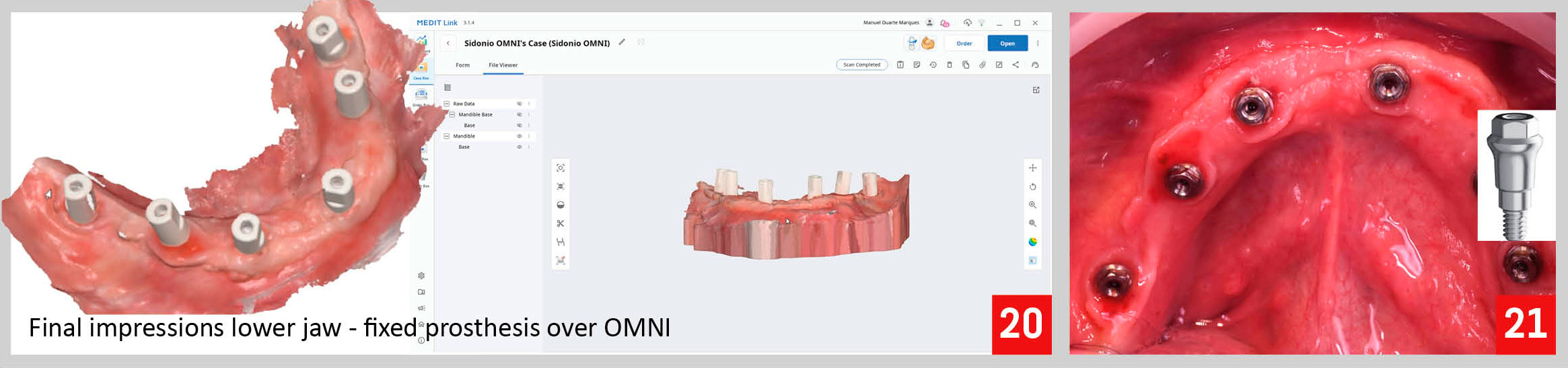
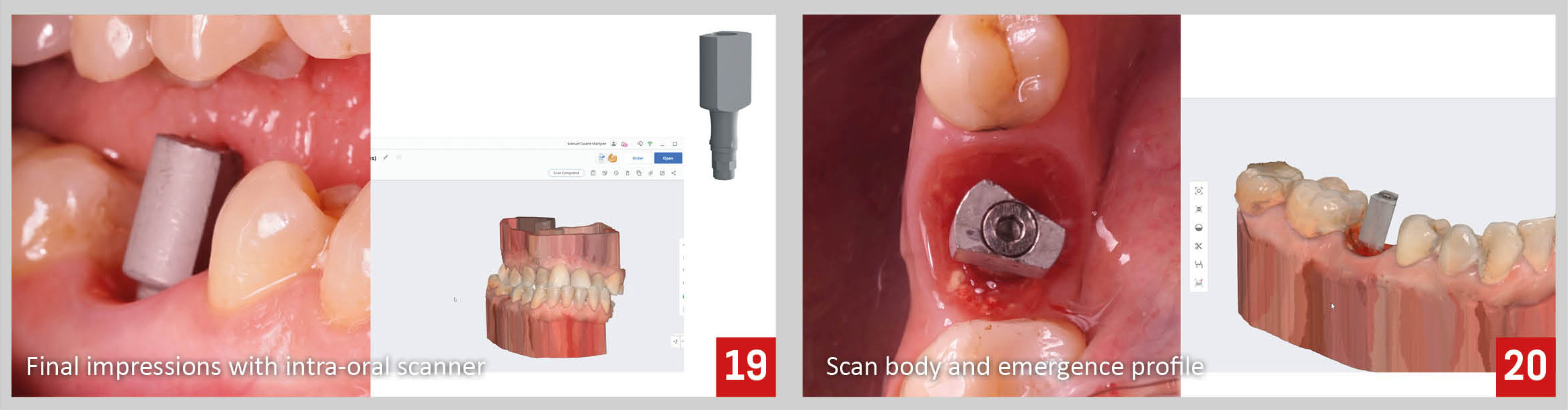
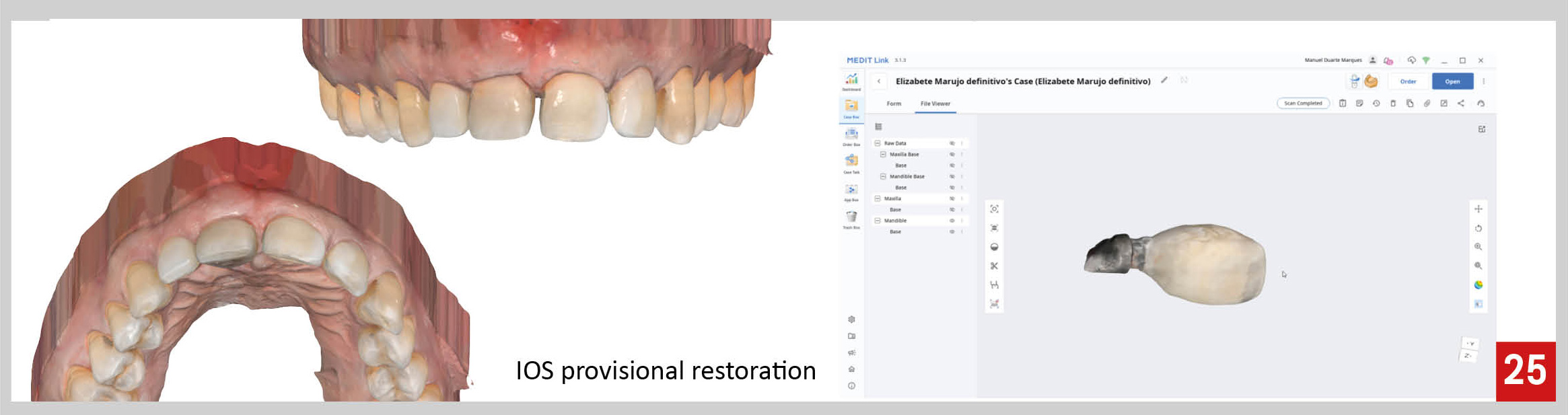
The final impressions were done digitally using an intra-oral scanner. The scanner allow not only the record of the implant position, but also, of the soft tissue anatomy, with great detail (Fig 19,20).
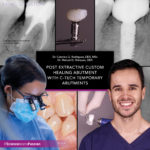
The final crown was fabricated fully digitally in monolithic zirconia. At the time of crown delivery, we could appreciate, in an oclusal view, a proper gingival thickness, and in a lateral view, a very natural soft tissue contour and maintenance of the interdental papilla (Fig. 21,22).