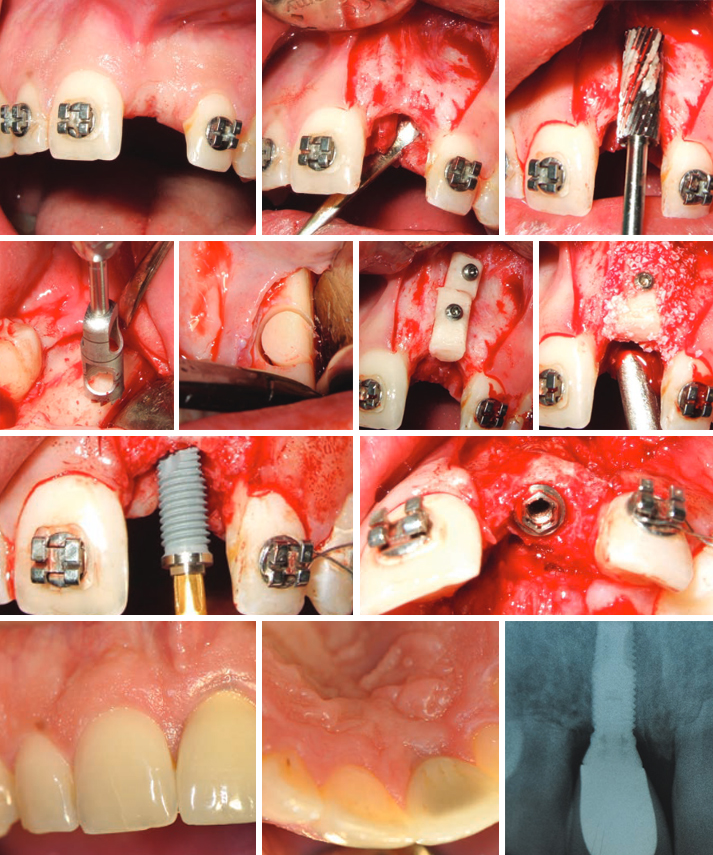
The aim of this study was to analyze clinical outcome of horizontal augmentation with autologous bone block grafts for the reconstruction of narrow edentulous ridge before implant placement. Eighteen partially edentulous patients, presenting insufficient bone width (less than 4mm) in the sites for implant placement were selected.
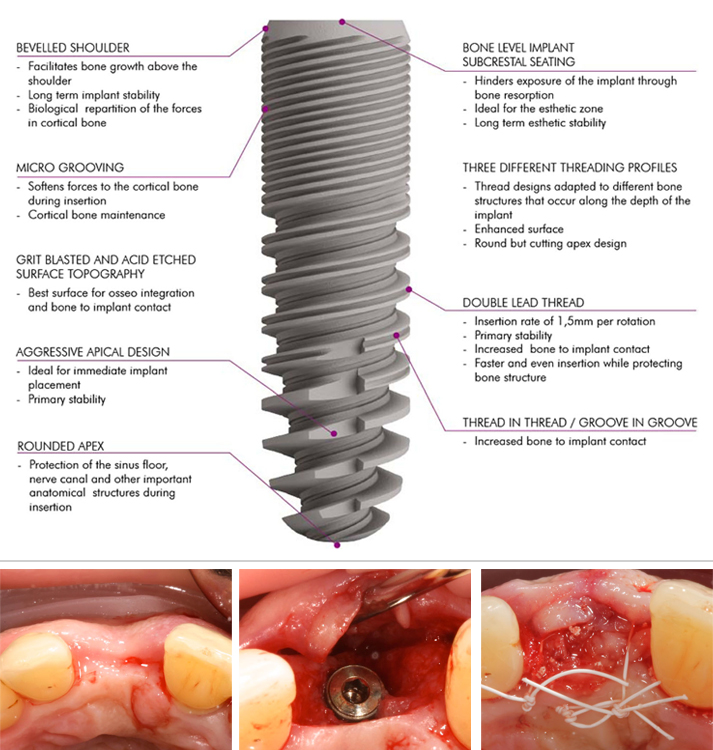
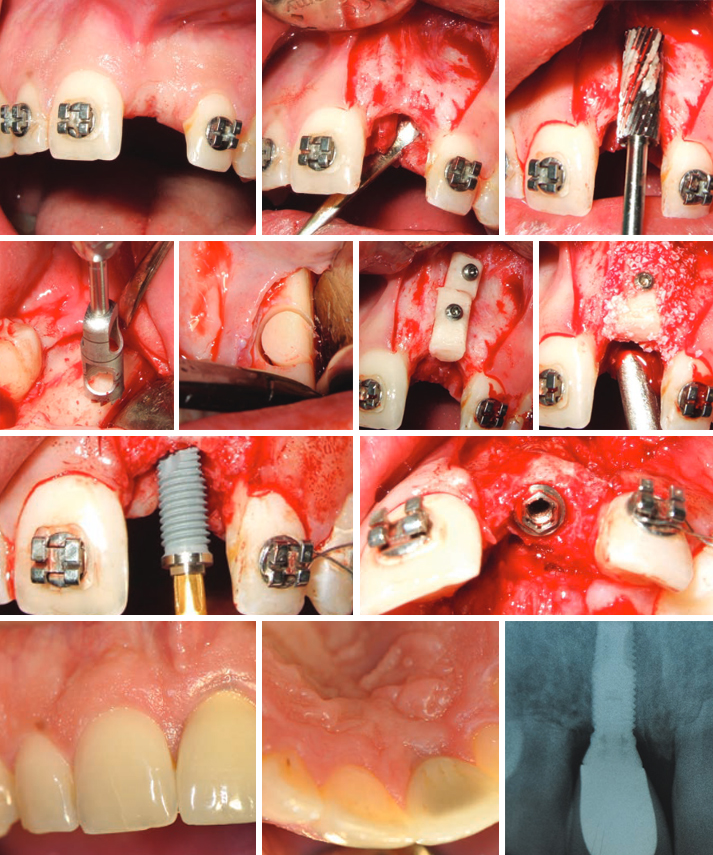
One or multiple cylindrical block grafts were harvested with trephine burrs from retromolar region and stabilized with titanium miniscrews. Fixed grafts were covered with deproteinised bovine bone mineral granules (DBBM) and collagen membrane (CM). The average amount of bone gain was 3,6 mm. One of the 24 block grafts was lost during the early healing period. Five months later, during the re-entry for implants placement, the gain of ridge width obtained were measured. All implants were placed in correct position and considered successfully integrated during the observation period. Three month after the implant placement prosthetic rehabilitation was started.
The mean follow up after prosthetic load has been 25,4 months.
This technique is reliable means for the correction of narrow edentulous ridge. Close contact between the bone graft and recipient bed surface ensure fast and intense vascularization and subsequent osseointegration of the graft. Adding bovine bone mineral and collagen membrane over bone block minimize resorption during healing.
In all cases all planned implants could be placed in the correct positions.
The mean duration of follow up of the implants was 25,4 months. Prosthodontics rehabilitation involved single crowns or bridges.
Not a single implant was lost during the observation period. All implants were successful both aesthetically and functionally.
References
1. Albrektsson T., Zarb G., Wothington P. & Ericsson A.R. (1986) The long-term efficacy of currently used dental implants: A review and proposed criteria of success. International Journal of Oral and Maxillofacial Implants 1:1-25.
2. Araujo, M.G., Sonohara, M., Hayacibara, R., Car- daropoli, G.
& Lindhe, J. (2002) Lateral ridge augmentation by the use of grafts comprised of autologous bone or a biomaterial. An experiment in the dog. Journal of Clinical Periodontology 29:1122–1131.
3. Buser, D., Dula, K., Belser, U. C., Hirt, H. P. & Berthold, H.
(1995) Localized ridge augmen- tation using guided bone regeneration. II. Surgical procedure in the mandible. International Journal of Periodontics and Restora- tive Dentistry 15,10–29.
4. Buser D., Dula K., Hirt H.P., & Schenk R. (1996) Localized ridge augmentation using autografts and barrier membranes: A clinical study with 40 partially edentulous patients. Journal of Oral and Maxillofacial Surgery 54:420-432
5. Buser, D., Dula, K., Hess, D., Hirt, H.P. & Belser, U.C. (1999) Localized ridge augmentation with autografts and barrier membranes. Periodontology 2000 19:151–163.
6. Buser, D., Ingimarsson, S., Dula, K., Lussi, A., Hirt, H. P. & Belser, U. C. (2002) Long-term stability of osseointegrated implants in aug- mented bone: a 5-year prospective study in partially edentulous patients. International Journal of Periodontics and Restorative Dentistry 22,109–117.
7. Chiapasco M, Romeo E & Vogel G. (1998) Three-dimensional reconstruction of a knife-edge edentulous maxilla by sinus elevation, onlay grafts and sagittal osteotomy of the anterior maxilla: preliminary surgical and prosthetic results. Journal of Oral and Maxillofacial Implants, 13:394-399
8. Chiapasco M., Abati S., Romeo E., Vogel G. (1999) Clinical outcome of autogenous bone blocks or guided bone regeneration with e-PTFE membranes for the reconstruction of narrow edentulous ridges. Clin Oral Impl Res 1999:10:278-288
9. Chiapasco, M., Zaniboni, M. & Boisco, M. (2006) Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants. Clin- ical Oral Implants Research 17 (Suppl.):136–159.
10. Cordaro, L., Amade, D. S. & Cordaro, M. (2002) Clinical results of alveolar ridge aug- mentation with mandibular block bone grafts in partially edentulous patients prior to implant placement. Clinical Oral Implants Research 13,103–111.
11. Cordaro, L., Torsello, F., Accorsi Ribeiro, C., Libera- tore, M. & Mirisola di Torresanto, V.M. (2010) Inlay– onlay grafting for three-dimensional reconstruction of the posterior atropic maxilla with mandibular bone. The International Journal of Oral and Maxillofacial Surgery 39:350–357.
12. Cordaro L., Torsello F., Morcavallo S, Mirisola di Torresanto V. (2011) Effect of bovine bone and collagen membranes on healing of mandibular bone blocks: a prospective randomized controlled study. Clin. Oral Impl. Res. 22,2011;1145–1150.
13. Ha ‘mmerle, C.H. & Karring, T. (1998) Guided bone regeneration at oral implant sites. Periodontology 2000 17:151–175.
14. Jensen SS, Aaboe M, Pinholt EM, Hjorting-Hansen E, Melsen F, Ruy- ter IE. Tissue reaction and material characteristics of four bone substitutes. Int J Oral Maxillofac Implants 1996:11:55– 66.
15. Kuboki, Y., Jin, Q., Kikuchi, M., Mamood, J. & Takita, H. (2002) Geometry of artificial ECM: sizes of pores controlling phenotype expression in BMP-induced osteogenesis and chondrogenesis. Connective Tissue Research 43:529–534.
16. Lekholm U & Zarb G.A. (1995) Patient selection and preparation. In: Tissue-integrated prostheses: Osseointegration in clinical dentistry. Pp. 199-209. Chicago: Quintessence
17. Machtei, E.E. (2001) The effect of membrane ex- posure on the outcome of regenerative procedures in humans: a meta-analysis. Journal of Perio- dontology 72:512–516.
18. Misch, C. M. (1997) Comparison of intraoral sites for onlay grafting prior to implant placement. Journal of Oral and
Maxillofacial Implants, 6:767-776
19. Maiorana, C., Beretta, M., Salina, S. & Santoro, F. (2005) Reduction of autogenous bone graft resorption by means of bio-oss coverage: a prospective study. International Journal of Periodontics and Restorative Dentistry 25:19–25.
20. McAllister, B.S. & Haghighat, K. (2007) Bone aug- mentation techniques. Journal of Periodontology 78:377–396.
21. Nkenke, E., Schultze-Mosgau, S., Radespiel-Tro ‘ger, M., Kloss, F. & Neukam, F.W. (2001) Morbidity of harvesting of chin grafts: a prospective study. Clinical Oral Implants Research 12:495–502.
22. Sander, L., Frandsen, E.V., Arnbjerg, D., Warrer, K. & Karring, T. (1994) Effect of local metronidazole application on periodontal healing following guided tissue regeneration. Clinical findings. Journal of Periodontology 65:914–920.
23. Schwarz F., Ferrari D., Balic E., Buser D., Becker J., Sager M. Lateral ridge augmentation using equine- and bovine-derived cancellous bone blocks: a feasibility study in dogs. Clin. Oral Impl. Res. 21,2010;904–912.
24. Simion M., Baldoni M., Rossi P. & Zaffe D. (1994) A comparative study of the effectiveness of a e-PTFE membranes with and without early exposure during healing period. International Journal of Periodontology and Restorative Dentistry 14:167-180
25. Von Arx, T & Buser, D. (2006). Horizontal ridge augmentation using autogenous block grafts and the guided bone regeneration technique with collagen membranes: a clinical study with 42 patients. Clinical Oral Implants Research 17:359–366