Rehabilitation of the jaw by means of immediate implantation and immediate restoration Digital workflow

Magazine PIP • Practical Implantology and Implant Prosthetics • August 2022 | Issue 4′
Rehabilitation of the jaw by means of immediate implantation and immediate restoration Digital workflow
Catarina G. Rodrigues, DDS, MSc – Manuel D. Marques, DDS – Raquel Bandeira, CDT
The success of any complex dental treatment depends on proper diagnostics and treatment planning. Digital treatment planning, prosthetic backward planning and guided implant surgery can help improve success rates and predictability of complex rehabilitations. The 3D information about the bone anatomy obtained by means of digital volume tomography (DVT) of the patient form the basis for successful treatment planning.

1. Frontal view with centric occlusion preoperative.
2. Preoperative close-up of the patient’s smile.
3. Image data for the preoperative intraoral scan.
4. Virtual simulation of the prosthetic reconstruction using 2D CAD software (Smile Cloud Biometrics; ADN3D Bioetch SRL).
5. Virtual planning of the shape and position of the anterior teeth according to the measurement criteria ..
6. … the red-and-white aesthetic, planned with the 2D Facial Smile design.
PROCEDURE
The DVT data is imported and processed by means of appropriate software in order to plan the implant positions. The planning data is then used to virtually design the drilling template for guided implant placement, which is then 3D printed and used for optimal positioning of the implants. The use of 2D dental CAD software enables the development of a face-related digital smile design. This two-dimensional data can then be imported into 3D CAD software to design 3D mock ups and immediate temporary restorations.
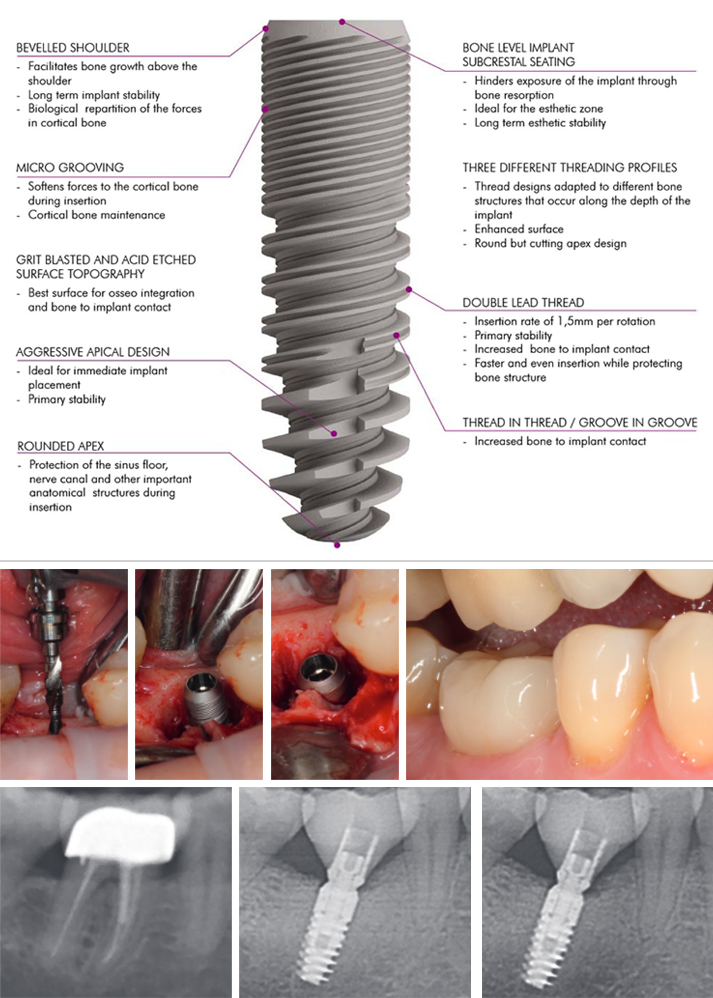
Advantages of immediate implantation
Immediate implantation of implant-supported prostheses is a predictable treatment option in the restoration of an edentulous jaw, as it can contribute to the preservation of the peri-implant soft and hard tissue and enable rapid patient assistance from an aesthetic and functional point of view. Important advantages of using digital technologies for the planning and execution of implant placement as well as for interim restoration are higher accuracy and precision in the fabrication of the overall rehabilitation, low invasiveness and optimal soft tissue shaping by the temporary prosthesis.
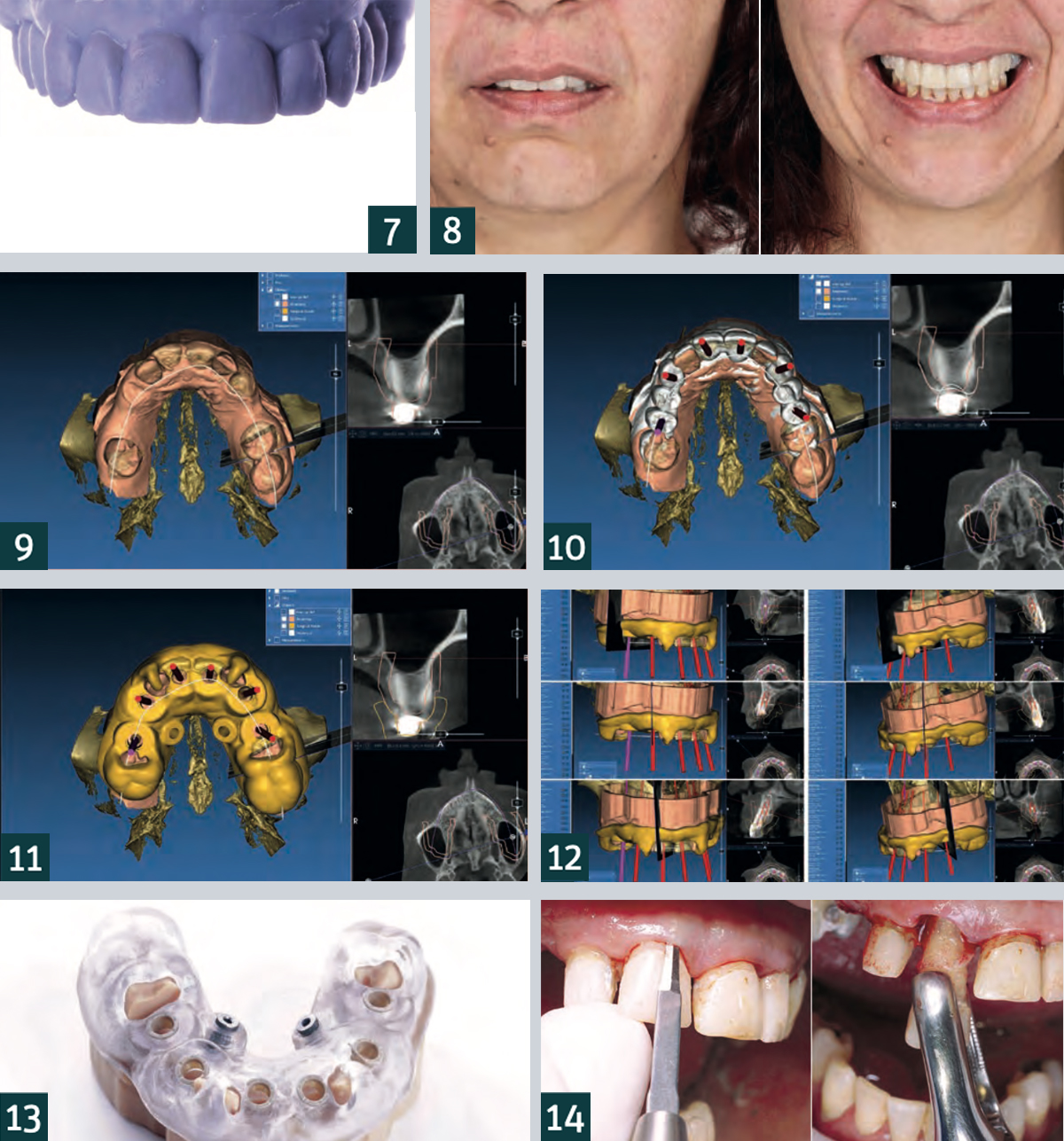
7. Frontal view of the 3D-printed model created from the diagnostic wax-up.
8. Frontal view of the preoperative mock up after transfer to the patient, checking the planning of the 2D facial smile design.
9. Superimposition of the STL data of the preoperative intraoral scan with the DVT data in the planning software (RealGUIDE, 3DIEMME).
10. Digital planning of the implants based on the anatomical situation and the previously planned prosthetic restoration.
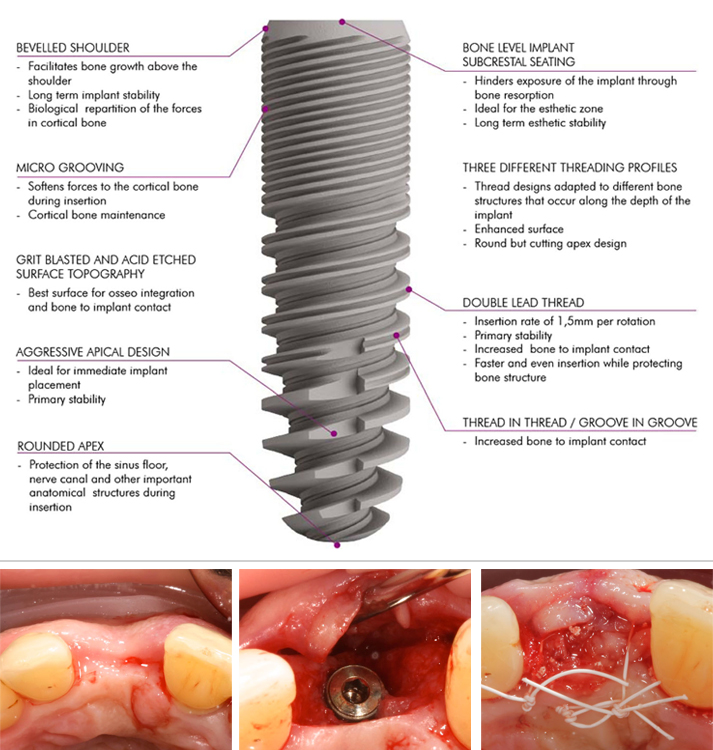
11. Once the final implant positions were determined, they were transferred to the surgical template design.
12. Planning of the implant positions.
13. Adjustment of the drilling template on the model.
14. Gentle extraction of the teeth not worth preserving in order to preserve the hard and soft tissue dimensions.
Patient case
The 40-year-old patient presented to our dental practice complaining in particular of difficulty eating and worsened aesthetics in the maxillary anterior region (Figs. 1, 2). The clinical and radiographic examination revealed a bilateral interdental gap in the maxillary posterior region. In addition to a fracture of tooth 13 at gingival level, insufficient amalgam and composite fillings as well as carious defects were diagnosed. There were also increased probing depths and generalised, radiographically visible, horizontal bone loss. After comprehensive diagnostics, it was decided, in consultation with the patient, to extract all of the upper anterior and posterior teeth, and proceed with immediate implantation of a total of eight implants and immediate provisional restoration with screw-retained dentures made of polymethyl methacrylate (PMMA). Intraoral scans (Fig. 3), a DVT and intraoral and extraoral photos (Fig. 4) were taken as part of preoperative diagnosis. In addition, a 2D digital facial smile design was created to enable planning of the position as well as the shape and size of the teeth for the future interim prosthesis (Figs. 5, 6). A digital diagnostic wax-up was then created using 3D CAD software and transferred to a corresponding model using 3D printing (Fig. 7).
Based on the model, a silicone index was created to enable the transfer of the acrylic resin trial restorations to the patient situation and 2D smile planning was undertaken for the patient’s mouth by means of a mock-up (Fig. 8). After adjusting and matching the shape and aesthetics of the anterior teeth, all three-dimensional data (DVT, preoperative intraoral scan and 3D mock-up) were imported into software (Fig. 9) and used to plan the implant position and fabricate the surgical guide (Figs. 10-12). In the patient case under discussion, a mostly fully-navigated implant placement was planned. Special guide sleeves adapted to the implant system were therefore integrated into the surgical template (Fig. 13). The surgical guide was stabilised with tooth support on teeth 16, 12, 22, 26 and 27 and with two palatal bone screws for which two screw channels had been integrated into the surgical guide. Implant preparation was initially fully navigated in the extraction sockets of teeth 13, 11, 21, 23 without opening and in region 15 and 25 with the formation of a mucoperiosteal flap.
After insertion of the six standard implants in the anterior region, the surgical template was removed, followed by extraction of teeth 16, 12, 22, 26 and 27 (Figs. 14-25). The placement of the two short implants was carried out freehand in region 16 and 26 after removal of the posterior teeth. All implant preparations were carried out according to the manufacturer’s recommended drilling protocol. The provisional prosthesis (Fig. 26) was screwed onto the six anterior implants via abutments and immediately loaded (Fig. 27). A postoperative X-ray was taken (Fig. 28). The patient is very satisfied with her new restoration, both aesthetically and functionally (Figs. 29-31).
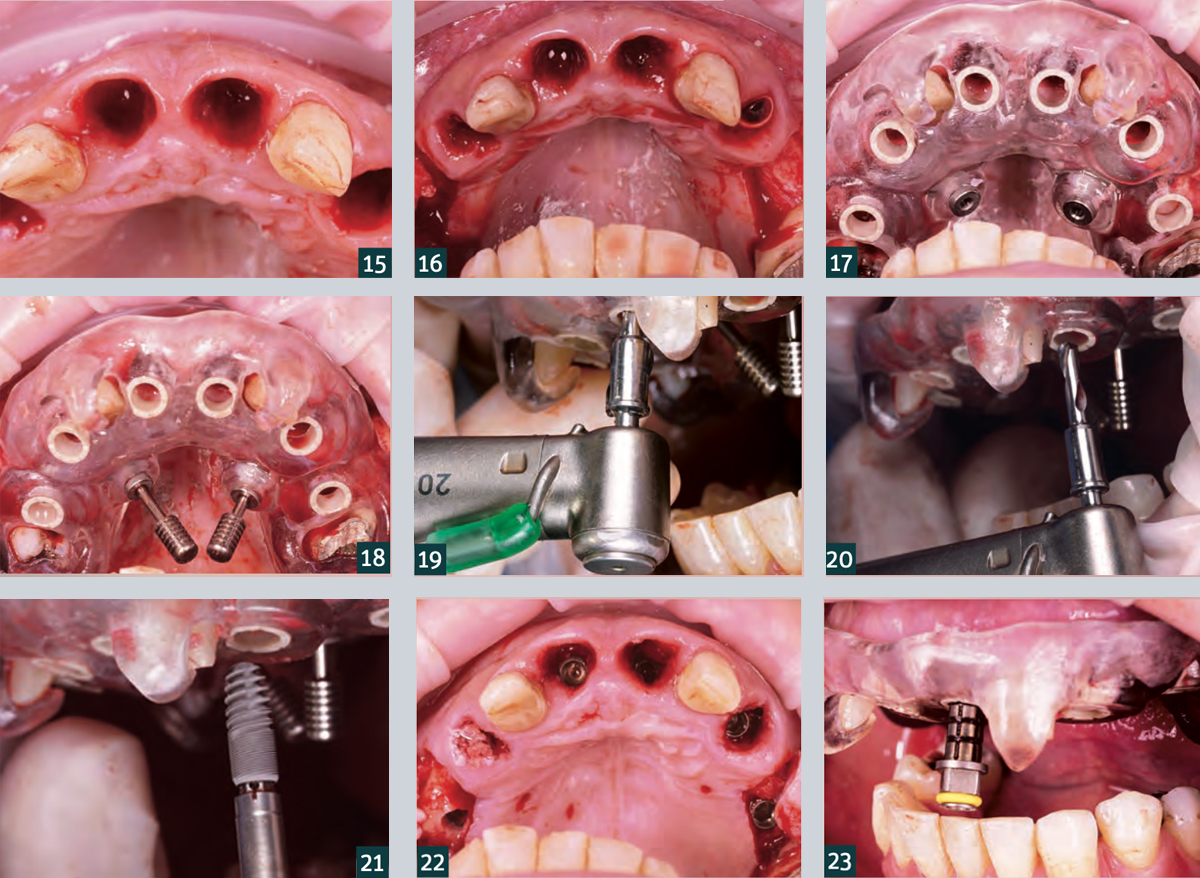 15. Teeth 12 and 22 were initially left in place to stabilise the surgical guide.
15. Teeth 12 and 22 were initially left in place to stabilise the surgical guide.
16. A full thickness flap was mobilised buccally in the premolar region of the quadrants to increase the soft tissue thickness.
17. Check the intraoral fit and stability of the surgical guide.
18. Additional stabilisation of the surgical guide via palatal fixation screws.
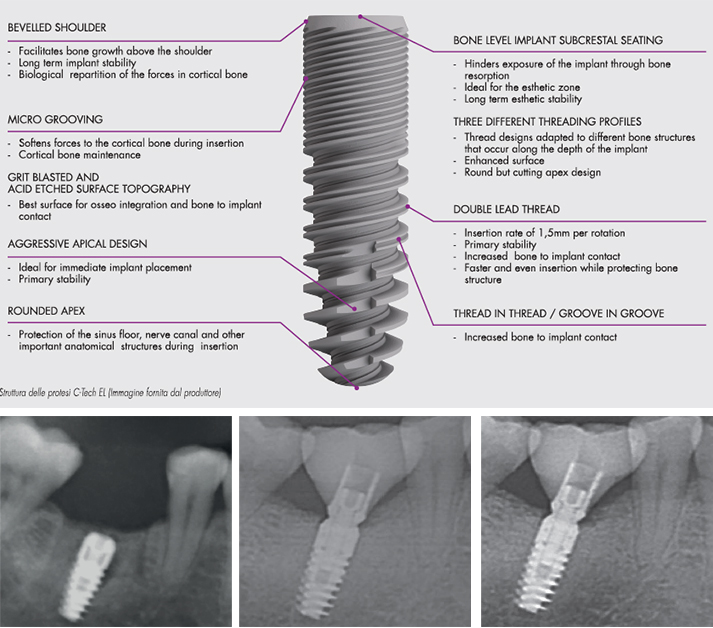
19. Template-guided implant drilling using the C-Guide drill..
20. … for C-Tech implants (C-Tech Implant, Bologna).
21. Template-guided implant placement (Esthetic Line implants, C-Tech Implants).
22. Occlusal view after placement of the six fully-navigated anterior implants.
23. Control: The markings on the transfer post correspond to the surgical guide sleeves.
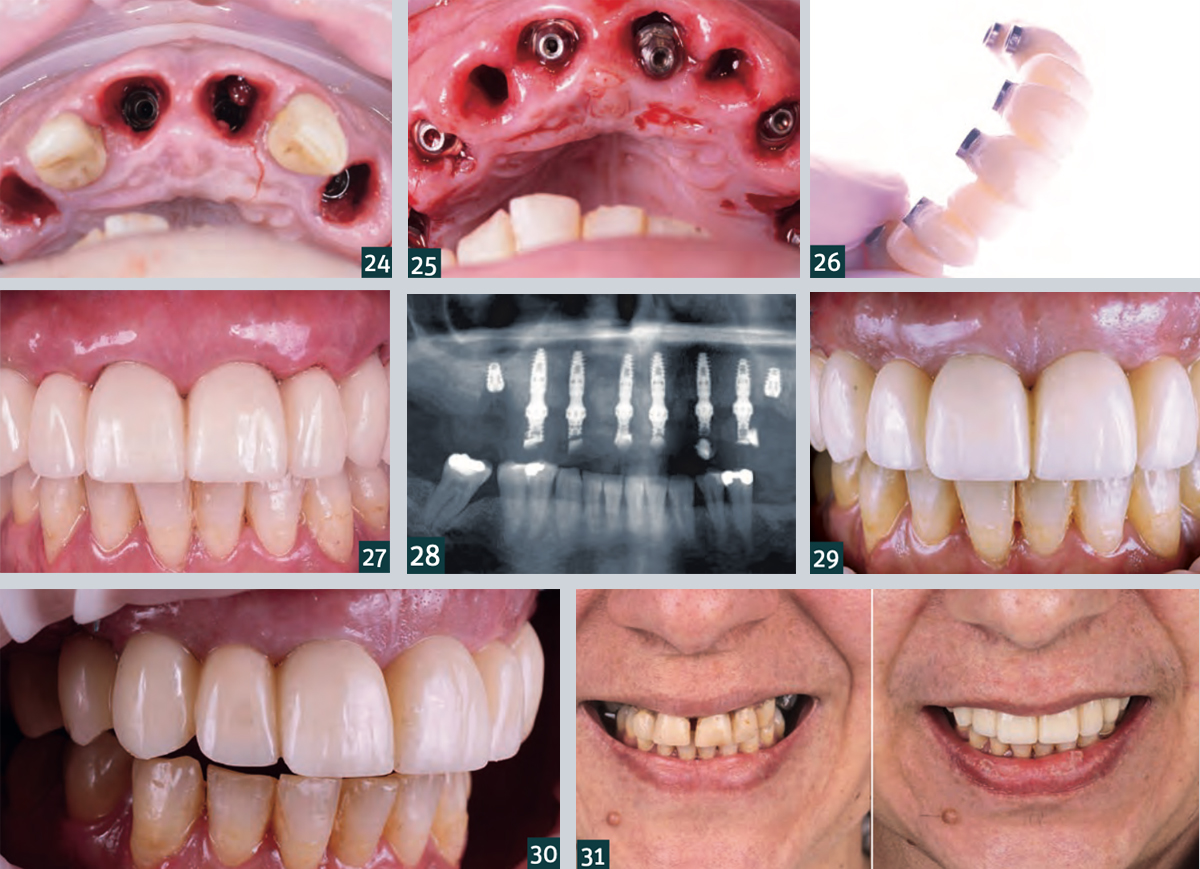
24. Occlusal view of the final implant position in apicocoronal direction (subcrestal positioning of the implants!).
25. Placement of the Multi Unit abutments.
26. Temporary denture made of PMMA.
27. Situation after insertion of the temporary denture with good postoperative soft tissue condition.
28. Radiograph showing postoperative check overview.
29. Intraoral situation one week after the procedure with…
30. … healing without complications and good soft tissue condition.
31. Comparison of the patient situation before (left) and one week after the intervention (right).