Стоматологические имплантаты стали надежным и прогнозируемым средством для замены отсутствующих зубов и сохранения зубного ряда у пациентов с адентией. Они могут восстановить здоровье ротовой полости, ее форму, функцию, жевание, артикуляцию и эстетику стоматологической системы — многолетняя успешность имплантации составляет более 90 % имплантатов у пациентов с полной [1,2] или частичной [3–6] адентией. Вариации в успешности имплантации зависят от техники проведения операции, протокола нагрузки, локализации имплантата и качества кости, например, о более низкой успешности имплантации сообщается при верхнечелюстной имплантации, в отличие от нижнечелюстной [7,8].
За последние десятилетия исследования стоматологических имплантатов привели к значительным изменениям хирургических и простетических протоколов.
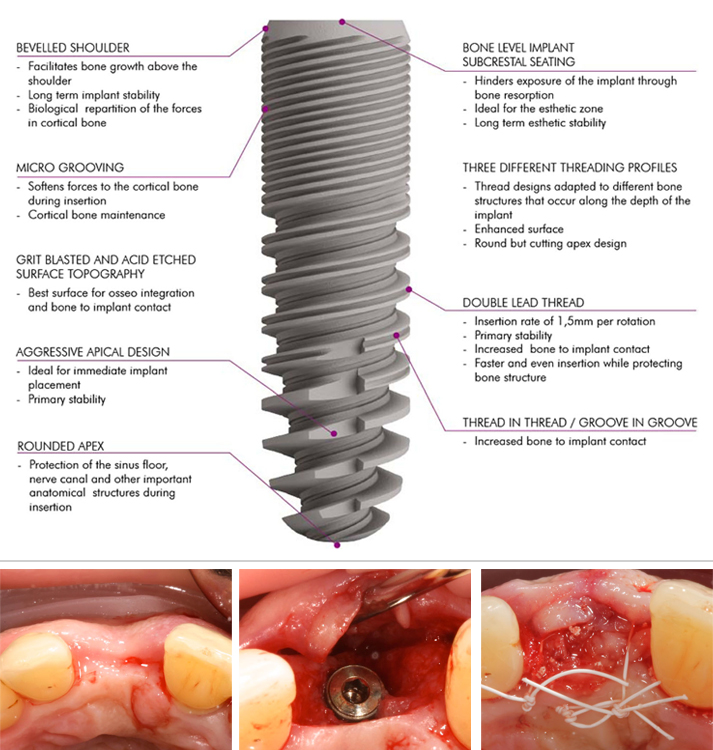
Что касается поверхности имплантатов, существует единогласное мнение о превосходстве поверхностей с шероховатостью/микротекстурой.
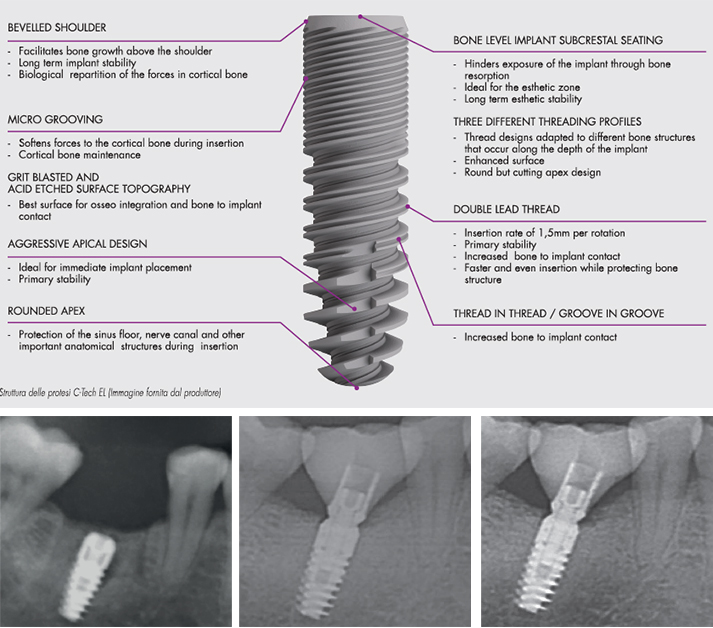
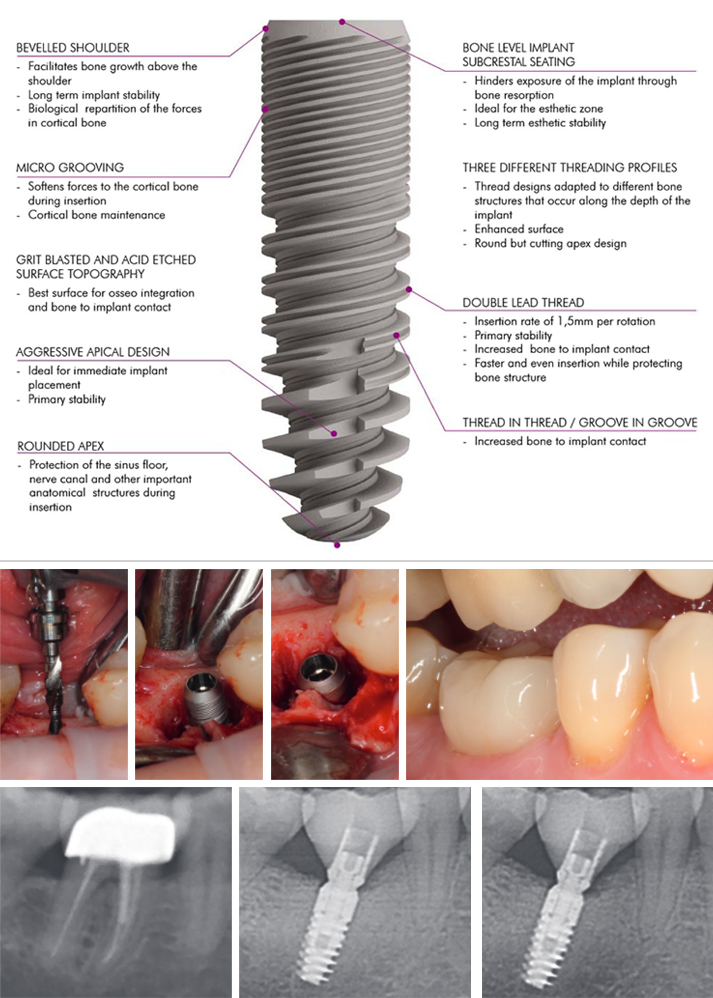
Другие способы улучшения поверхности имплантата включают конструкцию резьбы, длину имплантата и ширину имплантата. Конструкция имплантата должна обладать свойствами, которые наилучшим образом трансформируют натяжение и сдвигающее усилие во время жевания и минимизируют нежелательные составляющие силы.
Кроме того, для долгосрочной стабильности периимплантатной костной ткани, а также эстетически и функционально удовлетворительного стоматологического имплантата необходима стабильность соединения имплантата с абатментом, чтобы предотвратить трещины имплантата и ослабление винтов и сохранить стабильность периимплантатного уровня кости.
При конструкции, состоящей из двух частей, нельзя избежать расстояния или микрозазора между имплантатом и абатментом. Тем не менее меньший микрозазор иногда может образовываться в конструкциях с соединением платформ различных диаметров и в коническом соединении конусом Морзе, которые используются для передачи взаимодействия микрозазора и оси имплантата, а также для снижения микродвижений. Это может уменьшить поступательные движения жидкости десневой борозды и, следовательно, потерю альвеолярного гребня, даже если имплантаты установлены под альвеолярный гребень (ниже уровня костного гребня).
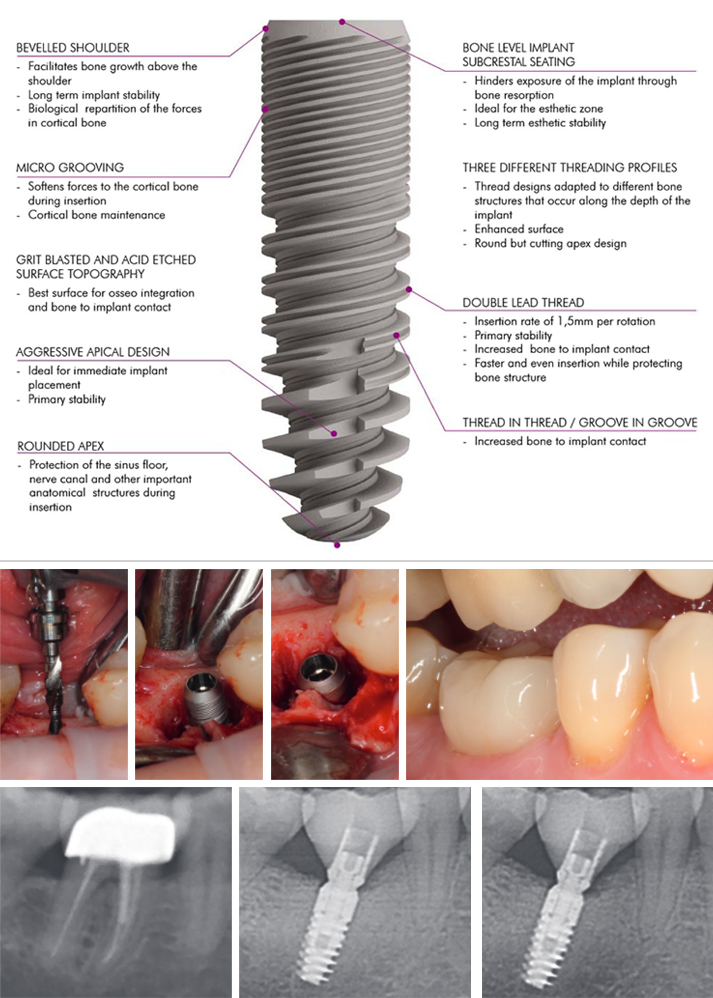
Цель этого ретроспективного исследования — описать клинические и радиологические результаты новой имплантационной системы с пескоструйно обработанной и протравленной кислотой топографией поверхности и коническим соединением Морзе имплантата и абатмента. Имплантаты были установлены в свежие и неповрежденные постэкстракционные лунки зубов верхней и нижней челюстей, которые не подлежали лечению, и наблюдались клинически и радиологически после среднего времени нагрузки на протяжении двух лет. Особое внимание было уделено поддержанию периимплантатного здоровья и стабильности периимплантатного уровня кости.
References
1. Albrektsson T, Dahl E, Enbom L, Engevall S, Engquist B, et al. (1988) Osseointegrated oral implants. A Swedish multicenter study of 8139 consecutively inserted nobelpharma implants. J Periodontol 59(5):287-296.
2. Spiekermann H, Jansen VK, Richter EJ (1995) A 10-year follow-up study of IMZ and TPS implants in the edentulous mandible using bar-retained overdentures. Int J Oral
Maxillofac Implants 10(2):231-243.
3. Nevins M, Langer B (1993) The successful application of osseointegrated implants to the posterior jaw: a long-term retrospective study. Int J Oral Maxillofac Implants 8(4):428-432.
4. Henry PJ, Laney WR, Jemt T, Harris D, Krogh PH, et al. (1996) Osseointegrated implants for single-tooth replacement: a prospective 5-year multicenter study. Int J Oral Maxillofac Implants 11(4):450-455.
5. Schmitt A, Zarb GA (1993) The longitudinal clinical effectiveness of osseointegrated dental implants for single-tooth replacement. Int J Prosthodont 6(2):197-202.
6. Fugazzotto PA, Gulbransen HJ, Wheeler SL, Lindsay JA (1993) The use of IMZ osseointegrated implants in partially and completely edentulous patients: success and failure rates of 2,023 implant cylinders up to 60+ months in function. Int J Oral Maxillofac Implants 8(6):617-621.
7. Misch CE (1990) Density of bone: effect on treatment plans, surgical approach, healing, and progressive boen loading. Int J Oral Implantol 6(2):23-31.
8. Albrektsson T, Lekholm U (1989) Osseointegration: current state of the art. Dent Clin North Am 33 (4):537-554.
9. Adell R, Lekholm U, Brånemark PI (1985) Surgical procedures. In: Brånemark PI, Zarb G, Albrektsson T (Eds.), Tissue Integrated Prostheses: Surgical Procedures, Quintessence Publishing Co, Chicago, USA, pp. 223-225.
10. Kohal RJ, LaRosa M, Patrick D, Hürzeler MB, Caffesse RG (1999) Clinical and histologic evaluation of submerged and nonsubmerged hydroxyapatite-coated im-plants: a preliminary study in dogs. Int J Oral Maxillofac Implants 14(6):824-834.
11. Evian CI, Kessler L, Axler J (1997) One-stage surgery with a nonsubmerged implant system. Compend Contin Educ Dent 18(11):1091-1094,1096-1098.
12. Ericsson I, Nilner K, Klinge B, Glantz PO (1996) Radio-graphical and histological characteristics of submerged and nonsubmerged titanium implants. An experimental study in the Labrador dog. Clin Oral Implants Res 7(1):20-26.
13. Chrcanovic BR, Albrektsson T, Wennerberg A (2015) Dental implants inserted in fresh extraction sockets versus healed sites: a systematic review and meta-analysis. J Dent 43(1):16-41.
14. Weiss CM, Weiss A, Rosenlicht J (2001) Root form implants. Treatment of total mandibular edentulism diagnosed for an overdenture. In: Weiss CM, Weiss A, (Eds.), Principles and Practice of Implant Dentistry, Mosby, St Louis, USA, pp. 147-168.
15. Fickl S, Zuhr O, Wachtel H, Stappert CF, Stein JM, et al. (2008) Dimensional changes of the alveolar ridge contour after different socket preservation techniques. J Clin Peri-odontol 35(10):906-913.
16. Vignoletti F, Matesanz P, Rodrigo D, Figuero E, Martin C, et al. (2012) Surgical protocols for ridge preservation after tooth extraction. A systematic review. Clin Oral Implants Res 23(5):22-38.
17. Lekovic V, Camargo PM, Klokkevold PR, Weinlaender M, Kenney EB, et al. (1998) Preservation of alveolar bone in extraction sockets using bioabsorbable membranes. J Periodontol 69(9):1044-1049.
18. Becker W, Becker B, Polizzi G, Bergstrom C (1994) Autogenous bone grafting of defects adjacent to implants placed into immediate extraction sockets in patients: a prospective study. Int J Oral Maxillofac Implants 9(4):389-396.
19. Artzi Z, Tal H, Dayan D (2001) Porous bovine bone mineral in healing of human extraction sockets: 2. Histo-chemical observations at 9 months. J Periodontol 72(2):152-159.
20. Iasella JM, Greenwell H, Miller RL, Hill M, Drisko C (2003) Ridge preservation with freeze-dried bone allograft and a collagen membrane compared to extraction alone for implant site development: a clinical and histologic study in humans. J Periodontol 74(7):990-999.
21. Araújo MG, Lindhe J (2005) Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol 32(2):212-218.
22. Evans CD, Chen ST (2008) Esthetic outcomes of immediate implant placements. Clin Oral Implants Res 19(1):73-80.
23. Chen ST, Darby IB, Reynolds EC, Clement JG (2009) immediate implant placement postextraction without flap elevation. J Periodontol 80(1):163-172.
24. Lang NP, Pun L, Lau KY, Li KY, Wong MC (2012) A systematic review on survival and success rates of implants placed immediately into fresh extraction sockets after at least 1 year. Clin Oral Implants Res 23(5):39-66.
25. Pagni G, Pellegrini G, Giannobile WV, Rasperini G (2012) Postextraction alveolar ridge preservation: biological basis and treatments. Int J Dent 2012:151030.
26. Tavarez RR, Calixto AM, Maia Filho EM, Bandeca MC, Firoozmand LM, et al. (2014) Atraumatic extraction, implant placement and immediate provisionalization. J Contemp Dent Pract 15(4):513-517.
27. Misch CE (1999) Implant design considerations for the posterior regions of the mouth. Implant Dent 8(4):376-386.
28. Binon PP (2000) Implants and components: entering the new millennium. Int J Oral Maxillofac Implants 15(1):76-94.
29. Trisi P, Rao W, Rebaudi A (1999) A histometric comparison of smooth and rough titanium implants in human low-density jawbone. Int J Oral Maxillofac Implants 14(5):689-698.
30. Steigenga JT, Shammari KF, Nociti FH, Misch CE, Wang HL (2003) Dental implant design and its relationship to long-term implant success. Implant Dent 12(4):306-317.
31. Niznick G (2000) Achieving Osseointegration in soft bone: The search for improved results. Oral Health 90:27-32.
32. O’Sullivan D, Sennerby L, Meredith N (2000) Measurements comparing the initial stability of five designs of dental implants: a human cadaver study. Clin Implant Dent Relat Res 2(2):85-92.
33. Sykaras N, Iacopino AM, Marker VA, Triplett RG, Woody RD (2000) Implant materials, designs, and surface topographies: their effect on osseointegration. A literature review. Int J Oral Maxillofac Implants 15(5):675-690.
34. Canullo L, Penarrocha OD, Soldini C, Mazzocco F, Penarrocha M (2015) Microbiological assessment of the implant-abutment interface in different connections: cross-sectional study after 5 years of functional loading. Clin Oral Implants Res 26(4):426-434.
35. Pozzi A, Tallarico M, Moy PK (2014) Three-year post-loading results of a randomised, con-trolled, split-mouth trial comparing implants with different prosthetic interfaces and design in partially posterior edentulous mandibles. Eur J Oral Implantol 7(1):47-61.
36. Ghanaati S, Lorenz J, Obreja K, Choukroun J, Landes C, et al. (2014) Nanocrystalline hydroxyl apatite-based material already contributes to implant stability after 3 months: a clinical and radiologic 3-year followup investigation. J Oral Implantol 40(1):103-109.
37. Ghanaati S, Barbeck M, Lorenz J, Stuebinger S, Seitz O (2013) Synthetic bone substitute material comparable with xeno-geneic material for bone tissue regeneration in oral cancer patients: First and preliminary histological, histomorpho-metrical and clinical results. Ann Maxillofac Surg 3(2):126-138.
38. Sailer I, Zembic A, Jung RE, Siegenthaler D, Holderegger C (2009) Randomized controlled clinical trial of customized zirconia and titanium implant abutments for canine and posterior single-tooth implant reconstructions: preliminary results at 1 year of function. Clinical Oral Implants Research 20(3):219-225.
39. Brägger U, Bürgin WB, Hämmerle CH, Lang NP (1997) Associations between clinical parameters assessed around implants and teeth. Clinical Oral Implants Research 8(5):412-421.
40. Berglundh T, Lindhe J, Ericsson I, Marinello CP, Liljenberg B, et al. (1991) The soft tissue barrier at implants and teeth. Clinical Oral Implants Research 2(2):81-90.
41. Berglundh T, Lindhe J, Jonsson K, Ericsson I (1994) The topography of the vascular systems in the periodontal and peri-implant tissues in the dog. Journal of Clinical Periodontology 21(3):189-193.
42. Moon IS, Berglundh T, Abrahamsson I, Linder E, Lindhe J (1999) The barrier between the keratinized mucosa and the dental implant. An experimental study in the dog. Journal of Clinical Periodontology 26(10):658-663.
43. Lindhe J, Berglundh T (1998) The interface between the mucosa and the implant. Periodontology 2000 17: 47-54.
44. Rieder D, Eggert J, Krafft T, Weber HP, Wichmann MG (2014) Impact of placement and restoration timing on single-implant esthetic outcome-a randomized clinical trial. Clin Oral Implants Res 27(2):e80-e86.
45. Romanos GE, Aydin E, Locher K, Nentwig GH (2014): Immediate vs. delayed loading in the posterior mandible: a split-mouth study with up to 15 years of follow-up. Clin Oral Implants Res 27(2):e74-e79.
46. Wagenberg B, Froum SJ (2014) Long-Term Bone Stability around 312 Rough-Surfaced Immediately Placed Implants with 2-12-Year Follow-Up. Clin Implant Dent Relat Res 17(4):658-666.
47. Javed F, Ahmed HB, Crespi R, Romanos GE (2013) Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interv Med Appl Sci 5(4):162-167.
48. Calvo GJL, Gomez MG, Aguilar SA, Mate SVJE, Abboud M (2014) Bone remodeling at implants with different configurations and placed immediately at different depth into extraction sockets. Experimental study in dogs. Clin Oral Implants Res 26(5):507-515.
49. Javed F, Almas K, Crespi R, Romanos GE (2011) Implant surface morphology and primary stability: is there a connection? Implant Dent 20(1):40-46.
50. Berberi A, Tehini G, Rifai K, Bou NEF, El ZN (2014) In vitro evaluation of leakage at implant-abutment connection of three implant systems having the same prosthetic interface using rhodamine B. Int J Dent 2014:351263.