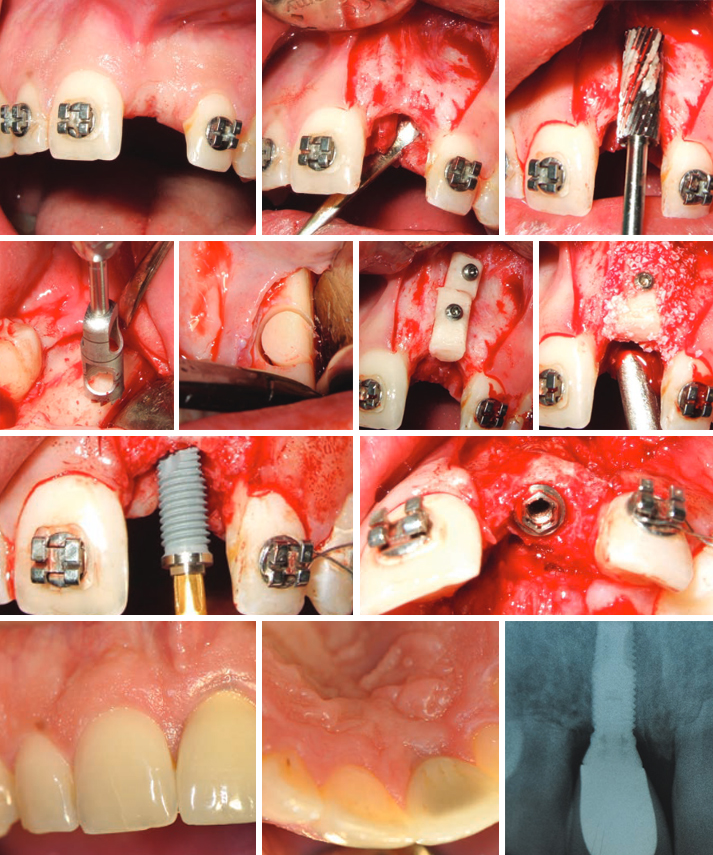
Целью этого исследования являлся анализ клинических результатов горизонтальной аугментации с аутологичным пересадочным костным блоком для восстановления узкой зубной дуги перед установкой имплантата. Были отобраны восемнадцать пациентов с частичной адентией, у которых недостаточная ширина кости (менее 4 мм) в местах установки имплантатов.
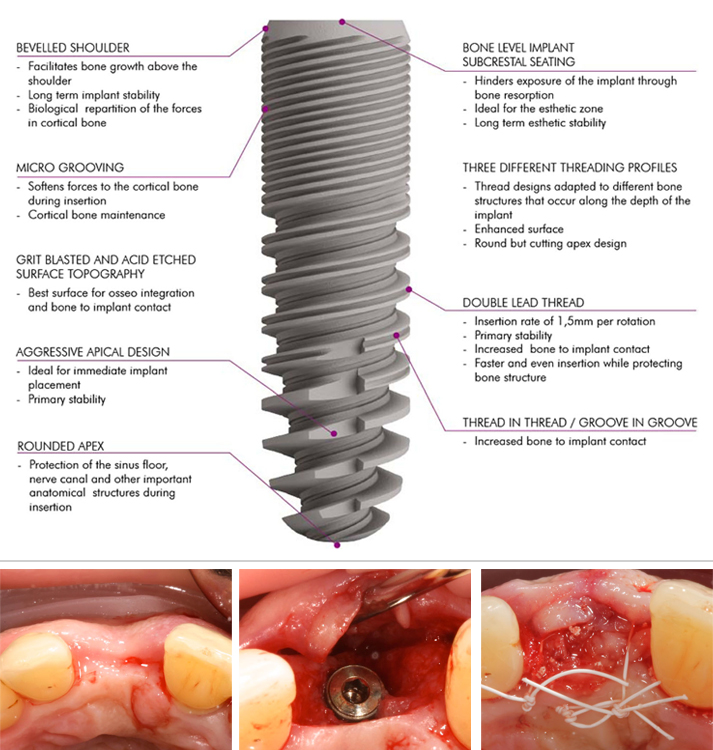
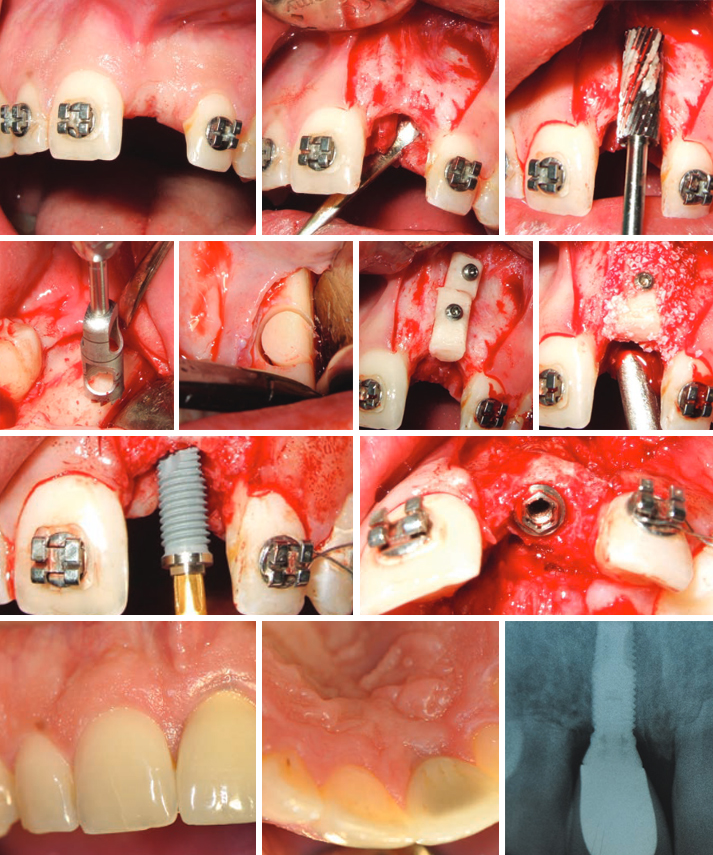
Один или несколько цилиндрических пересадочных костных блоков были собраны при помощи трепана с нижней челюсти и стабилизированы титановыми мини-винтами. Зафиксированные пересадочные блоки были покрыты безбелковой бычьей костной мембраной и коллагеновой мембраной. Среднее количество взятой кости составляло 3,6 мм. Один из 24 пересадочных блоков был потерян в начале периода восстановления. Пять месяцев спустя во время повторного визита для установки имплантатов ширина полученной зубной дуги была измерена. Все имплантаты были поставлены в правильные позиции и считались успешно интегрированными во время периода наблюдения. Через три месяца после установки имплантата было начато протезирование.
Среднее наблюдение после простетической нагрузки составляло 25,4 месяца.
Эта техника является надежным средством коррекции узкой зубной дуги с адентией. Плотный контакт между пересадочным костным блоком и поверхностью реципиентного ложа обеспечивает быструю и интенсивную васкуляризацию, а в последующем — остеоинтеграцию пересадочного костного блока. Добавление бычьего костного минерала и коллагеновой мембраны на пересадочный костный блок минимизирует рассасывание костных тканей во время выздоровления.
Во всех случаях все запланированные имплантаты могут быть установлены в правильных позициях.
Средняя длительность последующего наблюдения за имплантатами составляет 25,4 месяца. Зубное протезирование включало единичные коронки или мосты.
Во время периода наблюдения не был утрачен ни один имплантат. Все имплантаты были успешными как с точки зрения эстетики, так и с точки зрения функциональности.
References
1. Albrektsson T., Zarb G., Wothington P. & Ericsson A.R. (1986) The long-term efficacy of currently used dental implants: A review and proposed criteria of success. International Journal of Oral and Maxillofacial Implants 1:1-25.
2. Araujo, M.G., Sonohara, M., Hayacibara, R., Car- daropoli, G.
& Lindhe, J. (2002) Lateral ridge augmentation by the use of grafts comprised of autologous bone or a biomaterial. An experiment in the dog. Journal of Clinical Periodontology 29:1122–1131.
3. Buser, D., Dula, K., Belser, U. C., Hirt, H. P. & Berthold, H.
(1995) Localized ridge augmen- tation using guided bone regeneration. II. Surgical procedure in the mandible. International Journal of Periodontics and Restora- tive Dentistry 15,10–29.
4. Buser D., Dula K., Hirt H.P., & Schenk R. (1996) Localized ridge augmentation using autografts and barrier membranes: A clinical study with 40 partially edentulous patients. Journal of Oral and Maxillofacial Surgery 54:420-432
5. Buser, D., Dula, K., Hess, D., Hirt, H.P. & Belser, U.C. (1999) Localized ridge augmentation with autografts and barrier membranes. Periodontology 2000 19:151–163.
6. Buser, D., Ingimarsson, S., Dula, K., Lussi, A., Hirt, H. P. & Belser, U. C. (2002) Long-term stability of osseointegrated implants in aug- mented bone: a 5-year prospective study in partially edentulous patients. International Journal of Periodontics and Restorative Dentistry 22,109–117.
7. Chiapasco M, Romeo E & Vogel G. (1998) Three-dimensional reconstruction of a knife-edge edentulous maxilla by sinus elevation, onlay grafts and sagittal osteotomy of the anterior maxilla: preliminary surgical and prosthetic results. Journal of Oral and Maxillofacial Implants, 13:394-399
8. Chiapasco M., Abati S., Romeo E., Vogel G. (1999) Clinical outcome of autogenous bone blocks or guided bone regeneration with e-PTFE membranes for the reconstruction of narrow edentulous ridges. Clin Oral Impl Res 1999:10:278-288
9. Chiapasco, M., Zaniboni, M. & Boisco, M. (2006) Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants. Clin- ical Oral Implants Research 17 (Suppl.):136–159.
10. Cordaro, L., Amade, D. S. & Cordaro, M. (2002) Clinical results of alveolar ridge aug- mentation with mandibular block bone grafts in partially edentulous patients prior to implant placement. Clinical Oral Implants Research 13,103–111.
11. Cordaro, L., Torsello, F., Accorsi Ribeiro, C., Libera- tore, M. & Mirisola di Torresanto, V.M. (2010) Inlay– onlay grafting for three-dimensional reconstruction of the posterior atropic maxilla with mandibular bone. The International Journal of Oral and Maxillofacial Surgery 39:350–357.
12. Cordaro L., Torsello F., Morcavallo S, Mirisola di Torresanto V. (2011) Effect of bovine bone and collagen membranes on healing of mandibular bone blocks: a prospective randomized controlled study. Clin. Oral Impl. Res. 22,2011;1145–1150.
13. Ha ‘mmerle, C.H. & Karring, T. (1998) Guided bone regeneration at oral implant sites. Periodontology 2000 17:151–175.
14. Jensen SS, Aaboe M, Pinholt EM, Hjorting-Hansen E, Melsen F, Ruy- ter IE. Tissue reaction and material characteristics of four bone substitutes. Int J Oral Maxillofac Implants 1996:11:55– 66.
15. Kuboki, Y., Jin, Q., Kikuchi, M., Mamood, J. & Takita, H. (2002) Geometry of artificial ECM: sizes of pores controlling phenotype expression in BMP-induced osteogenesis and chondrogenesis. Connective Tissue Research 43:529–534.
16. Lekholm U & Zarb G.A. (1995) Patient selection and preparation. In: Tissue-integrated prostheses: Osseointegration in clinical dentistry. Pp. 199-209. Chicago: Quintessence
17. Machtei, E.E. (2001) The effect of membrane ex- posure on the outcome of regenerative procedures in humans: a meta-analysis. Journal of Perio- dontology 72:512–516.
18. Misch, C. M. (1997) Comparison of intraoral sites for onlay grafting prior to implant placement. Journal of Oral and
Maxillofacial Implants, 6:767-776
19. Maiorana, C., Beretta, M., Salina, S. & Santoro, F. (2005) Reduction of autogenous bone graft resorption by means of bio-oss coverage: a prospective study. International Journal of Periodontics and Restorative Dentistry 25:19–25.
20. McAllister, B.S. & Haghighat, K. (2007) Bone aug- mentation techniques. Journal of Periodontology 78:377–396.
21. Nkenke, E., Schultze-Mosgau, S., Radespiel-Tro ‘ger, M., Kloss, F. & Neukam, F.W. (2001) Morbidity of harvesting of chin grafts: a prospective study. Clinical Oral Implants Research 12:495–502.
22. Sander, L., Frandsen, E.V., Arnbjerg, D., Warrer, K. & Karring, T. (1994) Effect of local metronidazole application on periodontal healing following guided tissue regeneration. Clinical findings. Journal of Periodontology 65:914–920.
23. Schwarz F., Ferrari D., Balic E., Buser D., Becker J., Sager M. Lateral ridge augmentation using equine- and bovine-derived cancellous bone blocks: a feasibility study in dogs. Clin. Oral Impl. Res. 21,2010;904–912.
24. Simion M., Baldoni M., Rossi P. & Zaffe D. (1994) A comparative study of the effectiveness of a e-PTFE membranes with and without early exposure during healing period. International Journal of Periodontology and Restorative Dentistry 14:167-180
25. Von Arx, T & Buser, D. (2006). Horizontal ridge augmentation using autogenous block grafts and the guided bone regeneration technique with collagen membranes: a clinical study with 42 patients. Clinical Oral Implants Research 17:359–366