Dentista Moderno, Italy – October 2016 – Follow-up after two years to check the health of peri-implant tissues and bone stability of a number of cases with immediate post-extraction insertion of a recently developed bone implant system
Dentista Moderno, Italy • October 2016
Follow-up after two years to check the health of peri-implant tissues and bone stability of a number of cases with immediate post-extraction insertion of a recently developed bone implant system.First report
Jonas Lorenz University Hospital Frankfurt · Department of oral, maxillofacial and plastic surgery, Henriette Lerner HL DENTCLINIC, Robert A. Sader Goethe-Universität Frankfurt am Main · Center of Stomatology
and Shahram Ghanaati Goethe University of Frankfurt/Main; Universitätsmedizin der Johannes Gutenberg-Universität Mainz · Department for Oral, Craniomaxillofacial and Facial Plastic Surgery; Institute of Pathology
Introduction
Dental implants have become a reliable and predictable treatment method in dentistry to replace the tooth and prosthesis in case of edentulism. Therefore the oral health, shape, operation, chewing, articulation and aesthetics of the stomatognathic apparatus can be restored with a multi-year success rate of more than 90% in the case of implants set in completely or partially edentulous patients.
For the success of an implant in the long term it is necessary to meet some specific technical and constructive requirements. An additional factor that is essential for the long-term stability of peri-implant bone tissue and to ensure an aesthetically and functionally adequate dental implant is the stability of the implant-abutment connection, as it is inevitable that a space or micro-gap will be created between the implant and the abutment. Nevertheless, there will be a smaller micro-gap if the design is equipped with a cone Morse connection and platform switching, which transfer the micro-gap to the front of the implant axis and reduce micro-motion. Therefore, the pumping of sulcular fluid and, consequently, crestal bone loss can be reduced even when the implant is inserted under the crest (subcrestal).
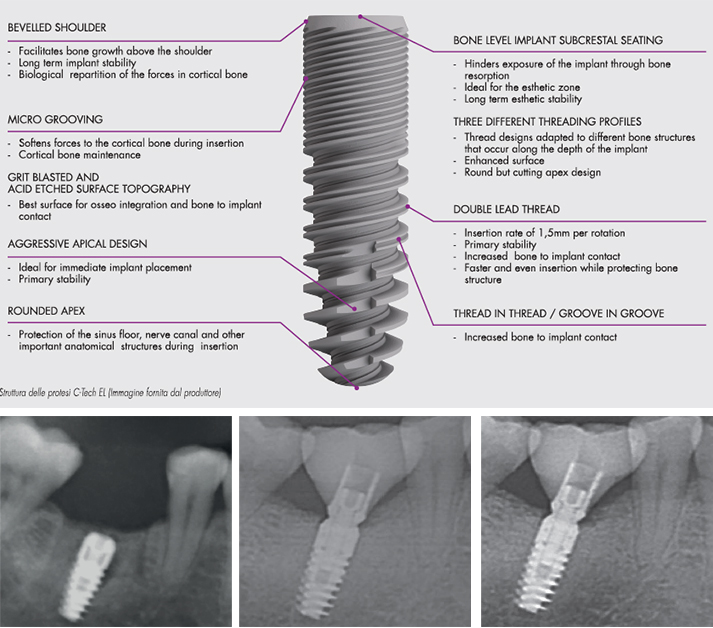
The purpose of the series of cases presented is to describe, for the first time, the clinical and radiological results after two years of immediate setting of 50 implants with a new sandblasted and acid-etched surface implant system and cone Morse connection.
During the observation period which averaged two years, none of the implants presented failures or acute or peri-implant infections. All implants had a sufficient amount of keratinised peri-implant soft tissue, reduced probing depths (2.25 mm on average) and good BOP (34%). After about two years of use, peri-implant bone level was stable and with an average bone loss of 0.83 mm.
With an average observation period of two years, the implant considered with immediate setting on the bone, rough surface and conical connection was shown to preserve the health status of the soft and hard peri-implant tissues. The parameters analysed are the same or better than comparable studies in the international literature.
References
1. Albrektsson, I; Dahl, E.; Enbom, L; Engevall, S.; Engquist, B.; Eriksson, A. R. et al. (1988): Osseointegrated oral implants. A Swedish multicenter study of 8139 consecutively inserted Nobelpharma implants. In: J. Periodontal 59 (5):287-296.
2. Spiekermann, H.; Jansen, V. K.; Richter, E. J. (1995): A 10-year follow-up study of IMZ and TPS implants in the edentulous mandible using bar-retained overdentures. In: Int J Oral Maxillofac Implants 10 (2):231 -243.
3. Nevins, M.; Longer, B. (1993): The successful application of osseointegrated implants to the posterior jaw: a long-term retrospective study. In: Int J Oral Maxillofac Implants 8 (4):428-432.
4. Henry, P. J.; Laney, W. R.; Jemt, T.; Harris, D.; Krogh, P. H.; Polizzi, G. et al. (1996): Osseointegrated implants for single-tooth replacement: a prospective 5-year multicenter study. In: Int J Oral Maxillofac Implants 11 (4):450-455.
5. Schmitt, A.; Zarb, G. A. (1993): The longitudinal clinical effectiveness of osseointegrated dental implants for single-tooth replacement. In: Int J Prosthodont 6 (2):197-202.
6. Fugazzotto, P. A.; Gulbransen, H. J.; Wheeler S. L.; Lindsay, J. A. (1993): The use of IMZ osseointegrated implants in partially and completely edentulous patients: success and failure rates of 2,023 implant cylinders up to 60+ months in function. In: Int J Oral Maxillofac Implants 8 (6):617-621.
7. Misch, C. E. (1990): Density of bone: effect on treatment plans, surgical approach, healing, and progressive boen loading. In: Int J Oral Impiantai 6 (2):23-31.
8. Albrektsson, T.; Lekholm, U. (1989): Osseointegration: current state of the art. In: Dent. Clin. North Am 33 (4):537-554.
9. Misch, C. E. (1999): Implant design considerations for the posterior regions of the mouth. In: Implant Dent 8 (4):376-386.
10. Binon, P. P. (2000): Implants and components: entering the new millennium. In: Int J Oral Maxillofac Implants 15 (1):76-94.
11. Trisi, R; Rao, W; Rebaudi, A. (1999): A histometric comparison of smooth and rough titanium implants in human low-density jawbone. In: Int J Oral Maxillofac Implants 14 (5):689-698.
12. Steigenga, Jennifer T.; al-Shammari, Khalaf R; Nociti, Francisco H.; Misch, Carl E.; Wang, Horn-Lay (2003): Dental implant design and its relationship to long-term implant success. In: Implant Dent 12 (4):306-317.
13. Niznick, G. (2000): Achieving Osseointegration in soft bone: The search for improved results. In: Oral Health, 2000;90:27-32.
14. O’Sullivan, D.; Sennerby, L; Meredith, N. (2000): Measurements comparing the initial stability of five designs of dental implants: a human cadaver study. In: Clin Implant Dent Relat Res 2 (2):85-92.
15. Sykaras, N.; Iacopino, A. M.; Marker, V. A.; Triplett, R. G.; Woody, R. D. (2000): Implant materials, designs, and surface topographies: their effect on osseointegration. A literature review. In: Int J Oral Maxillofac Implants 15 (5):675-690.
16. Canullo, Luigi; Penarrocha-Oltra, David; Soldini, Claudio; Mazzocco, Fabio; Penarrocha, Maria; Covani, Ugo (2015): Microbiological assessment of the implant-abutment interface in different connections: cross-sectional study after 5 years of functional loading. In: Clin Oral Implants Res 26 (4):426-434
17. Pozzi, Alessandro; Tallarico, Marco; Moy. Peter K. (2014): Three-year post-loading results of a randomised, controlled, split-mouth trial comparing implants with different prosthetic interfaces and design in partially posterior edentulous mandibles. In: Eur J Oral Impiantai 7 (1):47-61.
18. Ghanaati, Shahram; Lorenz, Jonas; Obreja, Karina; Choukroun, Joseph; Landes, Constantin; Sader, Robert A. (2014): Nanocrystalline hydroxyapatite-based material already contributes to implant stability after 3 months: a clinical and radiologic 3-year follow-up investigation. In: J Oral Impiantai 40 (1):103-109.
19. Ghanaati, Shahram; Barbeck, Mike; Lorenz, Jonas; Stuebinger, Stefan; Seitz, Oliver; Landes, Constantin et al. (2013): Synthetic bone substitute material comparable with xenogeneic material for bone tissue regeneration in oral cancer patients: First and preliminary histological, histomorphometrical and clinical results. In: Ann Maxillofac Sura 3 (2):126-138.
20. Sailer, I; Zembic, A; Jung, R; Siegenthaler, D; Holderegger, C; Hàmmerle, C. (2009): Randomized controlled clinical trial or customized zirconio and titanium implant abutments for canine and posterior single-tooth implant reconstructions: preliminary results at 1 year of function. In: Clinical Oral Implants Research; 20:219-225.
21. Bràgger, U; Burgin, W; Hàmmerle, C; Lang N. (1997): Associations between clinical parameters assessed around implants and teeth. In: Clinical Oral Implants Research; 8:412-421.
22. Tavarez, Rudys Rodolfo Jesus de; Calixto, Amanda Martins; Maia Filho, Etevaldo Matos; Bandeca, Matheus Coelho; Firoozmand, Leily Macedo; Gomes, Mario Gilson Nina; Malheiros, Adriana Santos (2014): Atraumatic extraction, implant placement and immediate provisionalization. In: J Contemp Dent Pract 15 (4):513-517.
23. Rieder, Dominik; Eggert, Jochen; Krafft, Tim; Weber, Hans-Peter; Wichmann, Manfred G.; Heckmann, Siegfried M. (2014): Impact of placement and restoration timing on single-implant esthetic outcome – a randomized clinical trial. In: Clin Oral Implants Res.
24. Romanos, Georgios E.; Aydin, Erhan; Locher, Kathrin; Nentwig, Georg-Hubertus (2014): Immediate vs. delayed loading in the posterior mandible: a split-mouth study with up to 15 years of follow-up. In: Clin Oral Implants Res.
25. Berberi, Antoine; Tehini, Georges; Rifai, Khaldoun; Bou Nasser Eddine, Farah; El Zein, Nabil; Badran, Bassam; Akl, Haidar (2014): In vitro evaluation of leakage at implant-abutment connection of three implant systems having the same prosthetic interface using rhodamine B. In: Int J Dent 2014:351263.





